Non-Surgical Periodontal Therapy: A Complete Beginner’s Guide to Gum Disease Treatment

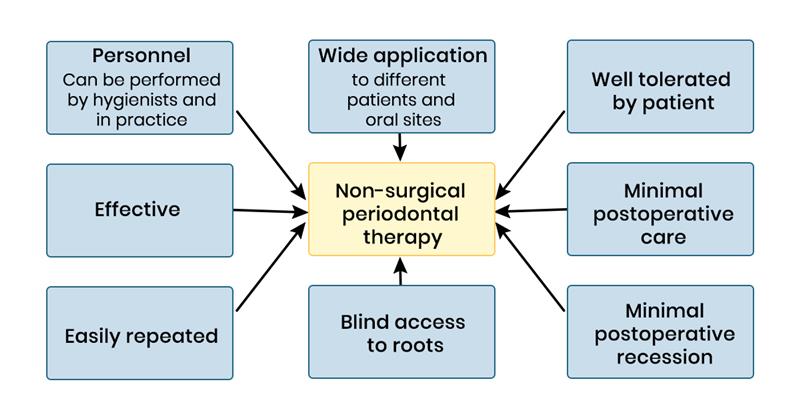
This guide is for those willing to take on periodontal disease without surgical intervention. It usually forms the first line of defense in treating gum diseases and saving teeth and, if well done, is quite effective.
In this blog, intended for both dental professionals and informed patients, we consider what NSPT is, why it is important, the main steps involved, and how you can integrate it into practice.
What is Non-Surgical Periodontal Therapy?
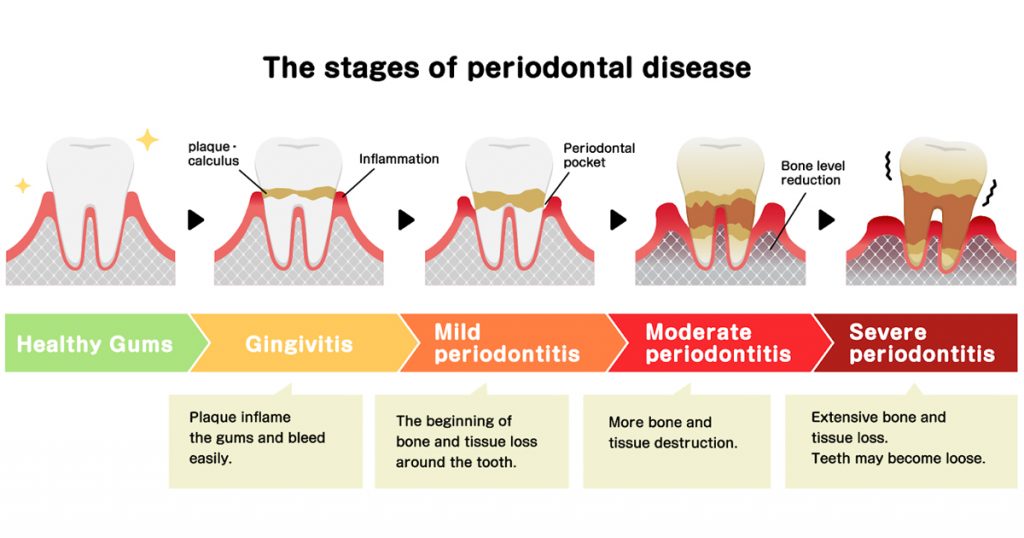
Non-surgical periodontal therapy consists of treatments directed at infection control, plaque and calculus removal from beneath the gumline, and risk factor modification in a non-invasive manner. Rather, the goals are to arrest disease progression, reduce pocket depth, and maintain natural dentition.
According to the source article-
- Remove and control supra- and sub-gingival microbial biofilms and calculus.
- Reduce or prevent inflammation.
- Eliminate or control both local and systemic risk factors contributing to periodontal disease.
If these goals are achieved, they would, in many cases, reduce or eliminate the need for surgical intervention.
Why Non-Surgical Therapy Is Important?
Several reasons explain why NSPT is so important:
- It also treats the root causes of periodontitis: biofilm, calculus, and risk factors, rather than just symptoms. It can be done in a typical dental office setting without the complexity and recovery time of surgery.
- Early intervention often provides a better long-term prognosis and helps maintain oral health and function.
- Many of the systemic conditions, which influence periodontal disease, are those conditions like diabetes or smoking, the control of which contributes to overall patient health.
The Seven-Step Protocol –
What follows is a modified version of the seven-step protocol from the reference article.
1. Controlling Systemic Risk Factors
Systemic factors such as uncontrolled diabetes, smoking, stress, immunodeficiency, and obesity impact periodontal disease progression and healing. Whenever possible, work with patients and their medical providers to control these risks before starting treatment. For instance, patients with poorly controlled diabetes should be stabilized before periodontal treatment commences.
2. Eradication of Local Risk Factors
Local risk factors include anatomical anomalies such as furcation, root grooves, mispositioned teeth, overhanging restorations, rough margins, and crowded teeth, all of which promote biofilm accumulation. Clearing these makes mechanical therapy more effective.
3. Behavior Modification Patient daily habits are critical.
Even the best mechanical therapy will fail without good oral hygiene. Interventions include:
It is suggested that both groups receive a detailed presentation on dental hygiene measures, including brushing, interdental cleaning, and tongue cleaning
Different preventive measures include the following: use of antiseptic rinses, where indicated.
- Individualized home-care instruction, depending on disease severity.
4. Scaling and Root Planning.
This is the clinical core of the world. The practitioner uses hands or ultrasonic instruments and/or other adjuncts to remove sub-gingival biofilm and calculus, and to smooth root surfaces. Evidence supports significant improvement in probing depths and clinical attachment levels when this step is executed nicely.
5. Antimicrobials
Clinicians may use systemic or local antimicrobials as adjuncts in selected cases, especially when risk factors or deep pockets are present. However, they should prescribe them judiciously to prevent antimicrobial resistance.
6. Re-evaluation
At 4–6 weeks following the active nonsurgical phase, reevaluate the patient’s periodontal status. Important measurements will include plaque index, bleeding on probing, probing depths, and attachment levels. Determine if additional nonsurgical therapy is needed or if surgical intervention or maintenance is required based on these findings.
7. Periodontal Maintenance
Long-term stability depends upon a customized maintenance plan. Frequent follow-ups, professional cleaning, and patient compliance are imperative in preventing relapse. In many patients treated for chronic periodontitis, 3-month intervals are considered standard, though period lengths may vary based on risk.
Practical Tips for Implementation:
- Use quality dental instruments and dental materials engineered for sub-gingival cleaning and root debridement.
- Make sure you’re stocking the right dental products for hygiene and maintenance-interdental brushes, antiseptic rinses, etc.
- Educate the patients regarding the effects of lifestyle factors-smoking, diabetes and stress-on their periodontal health.
- Devote sufficient time to scaling and root planning, don’t hurry through this important step.
- Document baseline and follow-up periodontal charting so you can track progress and decide on the next steps scientifically.
It is important to recognize when to refer for specialist surgical intervention if pockets remain deep (>5–6mm) or furcation involvement is present.
Common Misconceptions:
- If I do scaling and root planning, the job is done.
While scaling and root planning are important, they are not sufficient. Maintenance, risk factor control, and good home care are also important.
- Antibiotics fix the problem.
Antibiotics do not replace mechanical debridement and are indicated only in selected cases.
- Deep pockets always require surgery
Not always. Many moderate pockets respond to thorough NSPT. However, pockets with complex anatomy or furcation’s may require surgery.

Conclusion
Non-surgical periodontal therapy represents a cornerstone in modern periodontics. If performed systematically, including control of risk factors and patient behavioral modification, mechanical debridement, and supportive care, it can lead to very good results and significantly reduce indications for surgery.
As dental professionals, incorporating NSPT into your practice involves bringing together excellent technique, high-quality dental instruments and materials, and patient collaboration. For patients, NSPT offers a less invasive path to improved gum health, preserved teeth, and better overall health.
FAQs
Q1. How long after scaling and root planning should I see improvement?
You can expect a reduction in inflammation and bleeding within 4–6 weeks. Significant changes in probing depth take a bit longer but start to appear at the reevaluation phase.
Q2. What role do dental materials play in NSPT?
Other dental materials, such as antiseptic rinses, local delivery antimicrobials, and home-care aids, supplement mechanical therapy and support the maintenance of the therapeutic effect.
Q3. Can patients with uncontrolled diabetes still undergo NSPT?
Yes-but ideally after better metabolic control is achieved. Poorly controlled diabetes is associated with delayed healing and a greater risk of periodontal disease progression.
Q4. If a patient smoke – is NSPT still worthwhile?
Absolutely, smoking considerably diminishes the effectiveness of NSPT. Smoking cessation must be addressed as part of the therapy plan.
Q5. After NSPT, how often should maintenance visits be scheduled?
Typically, every 3 months patients should be treated for chronic or aggressive periodontitis. The interval may be longer for stable patients with low-risk profiles.



No Comment