Paediatric Pulp Therapy: Guidelines & Best Materials (Pulpotomy / Pulpectomy)
Introduction to Pediatric Pulp Therapy
In children, caries reaches the pulp fast because primary teeth have thinner enamel, dentin and larger pulp chambers. When the pulp is inflamed or infected, the aim is simple: keep the tooth comfortable, functional, and in place until natural exfoliation.

Saving a primary tooth helps:
- Maintain arch length and space for the permanent successor
- Preserve chewing efficiency and speech development
- Avoid early extractions and space maintainers
- Reduce pain, infection, and dental anxiety
Pulpotomy
Pulpotomy is a vital pulp therapy procedure performed when inflammation is limited to the coronal pulp, and the radicular pulp remains healthy.
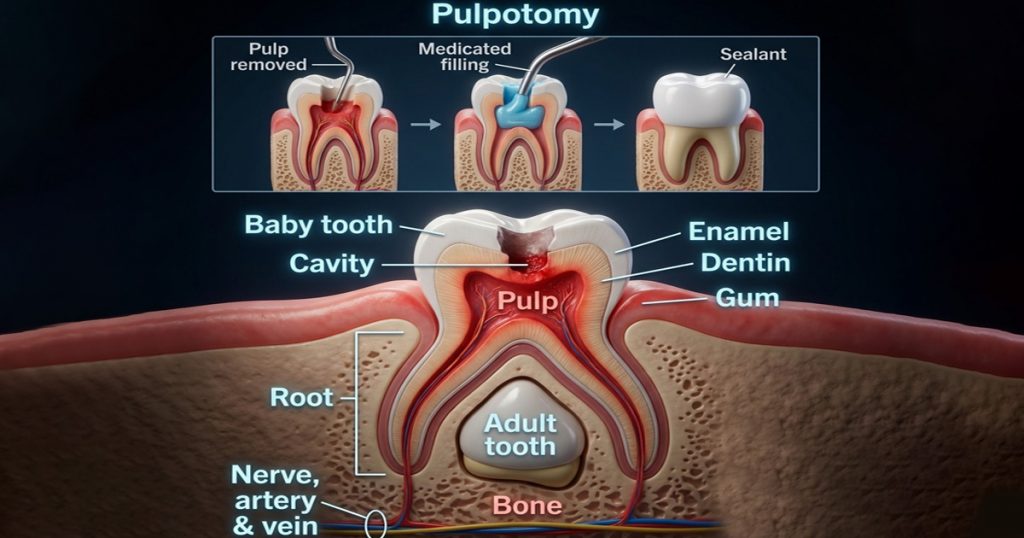
- The infected coronal pulp is removed
- Radicular pulp is preserved and treated with a medicament
- Mainly indicated in vital primary teeth with deep caries
- Success depends on proper diagnosis, hemostasis and a good coronal seal
Pulpectomy
Pulpectomy is a non-vital pulp therapy procedure where both coronal and radicular pulp tissues are completely removed.
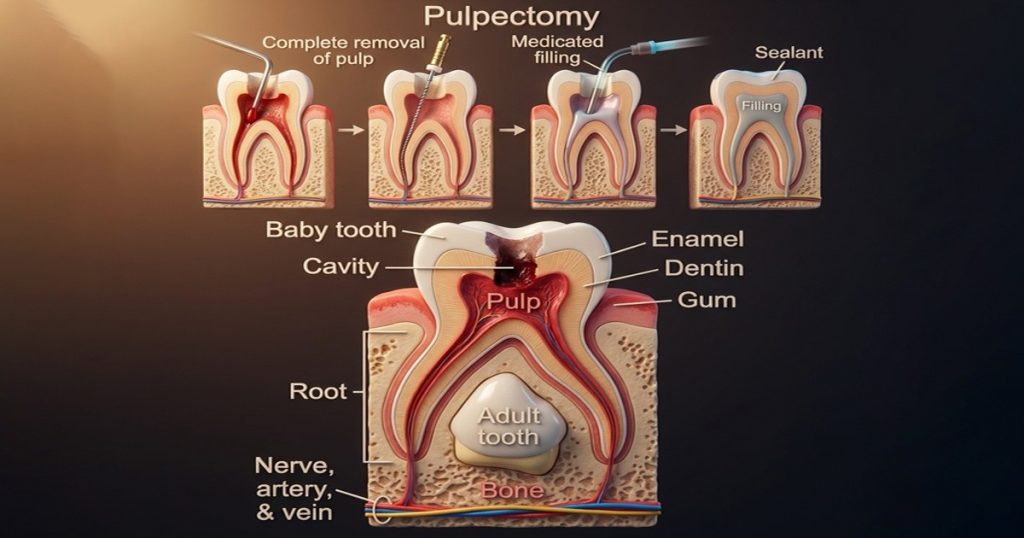
- Indicated when the pulp is necrotic or irreversibly inflamed
- The canals are cleaned, shaped, and obturated with a resorbable material
- Helps retain the primary tooth when extraction is not ideal
- Requires good isolation and child cooperation
Indications for Pulpotomy vs Pulpectomy
The choice depends on pulp status and clinical/radiographic signs.

Pulpotomy (Vital pulp therapy) – do when:
- Caries exposure occurs, but radicular pulp is still healthy
- Bleeding is bright red and controllable within a few minutes
- No signs of swelling, sinus tract, or furcation/periapical pathology
- Tooth is restorable and the child can return for follow-ups
Common case: deep caries with mechanical exposure during caries removal, no abscess.
Pulpectomy (Non-vital pulp therapy) – do when:
- Pulp is necrotic or irreversibly inflamed
- Signs like:
- Spontaneous pain / night pain history
- Swelling, sinus tract, tenderness to percussion
- Furcation radiolucency (especially in primary molars)
- Bleeding is uncontrolled, dark, or there is suppuration on access
- Tooth is restorable and expected to remain in mouth long enough to justify treatment
Common case: primary molar with furcation radiolucency and sinus tract.
Step-by-step Clinical Guidelines
A) Pulpotomy (Primary tooth)
Goal: remove coronal pulp, keep radicular pulp healthy, seal well.
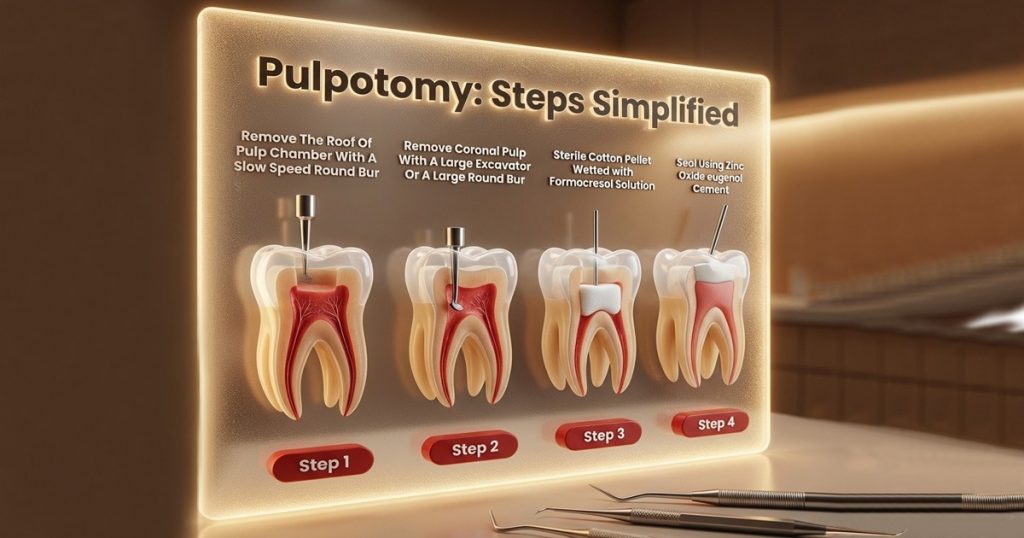
Steps:
- Local Anesthesia + rubber dam isolation
- Remove caries, access pulp chamber
- Remove coronal pulp completely
- Achieve hemostasis (gentle pressure with moist cotton pellet)
- Place pulpotomy medicament (best options below)
- Seal with base/liner
- Restore with a good seal (stainless steel crown for most primary molars is strongly preferred)
Quick clinical tips:
- If bleeding doesn’t stop or looks unhealthy → switch to pulpectomy or consider extraction based on restorability.
- Success depends heavily on the final seal and full coverage restoration.
B) Pulpectomy (Primary tooth)
Goal: remove infected pulp from canals, disinfect, fill with resorbable material, seal.
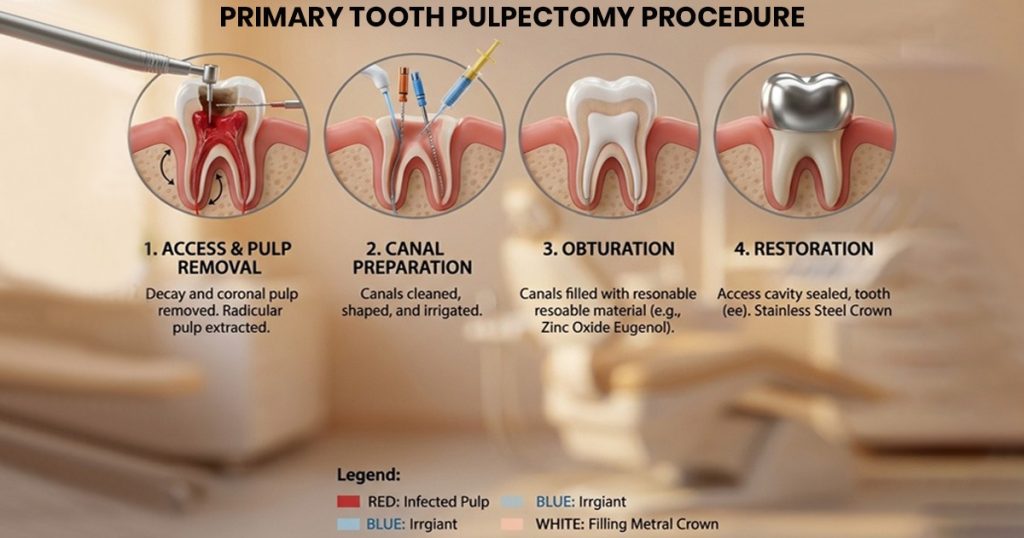
Steps:
- LA + rubber dam isolation
- Access and remove coronal pulp
- Find canals, extirpate radicular pulp
- Irrigate gently (avoid extrusion)
- Minimal shaping—primary canals are thin and fragile
- Dry canals
- Obturate with resorbable paste (options below)
- Restore with a tight coronal seal (SSC for most posterior teeth)
Quick clinical tips:
- Over-instrumentation and over-irrigation are common mistakes. Keep it gentle and controlled.
- If the child can’t tolerate long chair time, consider simplified approaches (see “Recent advances”).
Best Materials Used in Modern Practice
Best pulpotomy materials:

- Calcium silicate cements are widely preferred today because they’re more biocompatible and support healing.
- MTA (Mineral Trioxide Aggregate)
- Strong clinical track record, high success
- Excellent seal, encourages dentin bridge formation
- Downsides: cost, handling, potential discoloration (varies by type)
- Biodentine
- Similar bioactivity to MTA
- Faster setting and easier handling in many cases
- Good option where you want a smoother workflow
Other commonly used options (still seen in practice)
- Ferric sulfate
- Great for hemostasis and quick application
- Works well when isolation and seal are good
- Formocresol
- Historically popular
- Use has reduced due to safety concerns and preference for bioactive materials
Best pulpectomy obturation materials (primary teeth):
You want a material that:
- Is antibacterial
- Seals well
- Resorbs along with the roots (or at least doesn’t interfere with exfoliation)
Common choices:
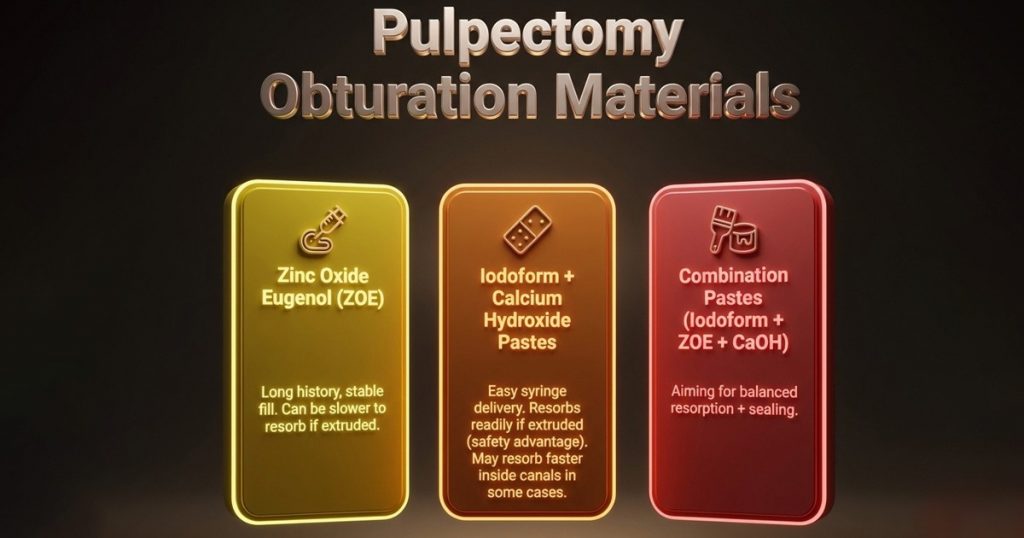
- Zinc oxide eugenol (ZOE)
- Long history, stable fill
- Can be slower to resorb if extruded
- Iodoform + calcium hydroxide pastes (e.g., Vitapex/Metapex-type)
- Easy syringe delivery
- Resorbs readily if extruded (safety advantage)
- May resorb faster inside canals in some cases
- Combination pastes (iodoform + ZOE + CaOH)
- Aiming for balanced resorption + sealing
Comparing Traditional vs Newer Materials (Simple & clear)
Pulpotomy: Formocresol vs MTA/Biodentine:
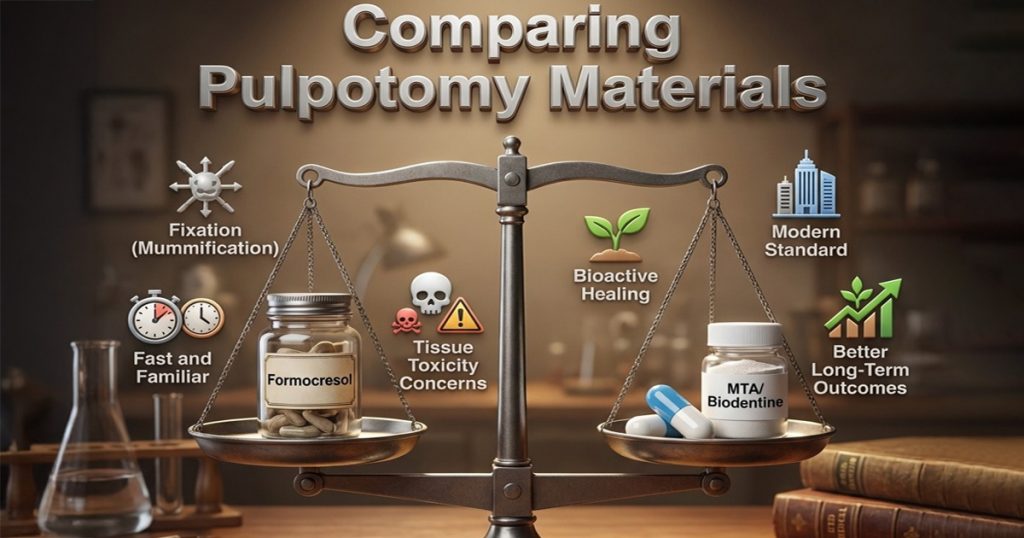
- Formocresol
- Works by fixation (mummification)
- Fast and familiar
- Concerns: tissue toxicity / systemic exposure discussions
- MTA / Biodentine
- Bioactive: supports healing and hard tissue formation
- Typically shows better long-term outcomes in many studies
- More “modern standard” in many clinics
Pulpectomy: ZOE vs Iodoform pastes:

- ZOE
- Strong long-term presence in canals
- Good seal, but extruded material may persist
- Iodoform pastes
- Faster resorption if overfilled
- Very convenient delivery
- Possible early resorption within canals in some cases
Practical selection mindset:
- Need durability for a tooth expected to stay longer → often ZOE or combination paste
- High chance of minor overfill / short roots / anxious child → iodoform paste can be forgiving
Challenges in Paediatric Pulp Therapy (Real-world)
Even with perfect technique, paediatric cases have their own hurdles:
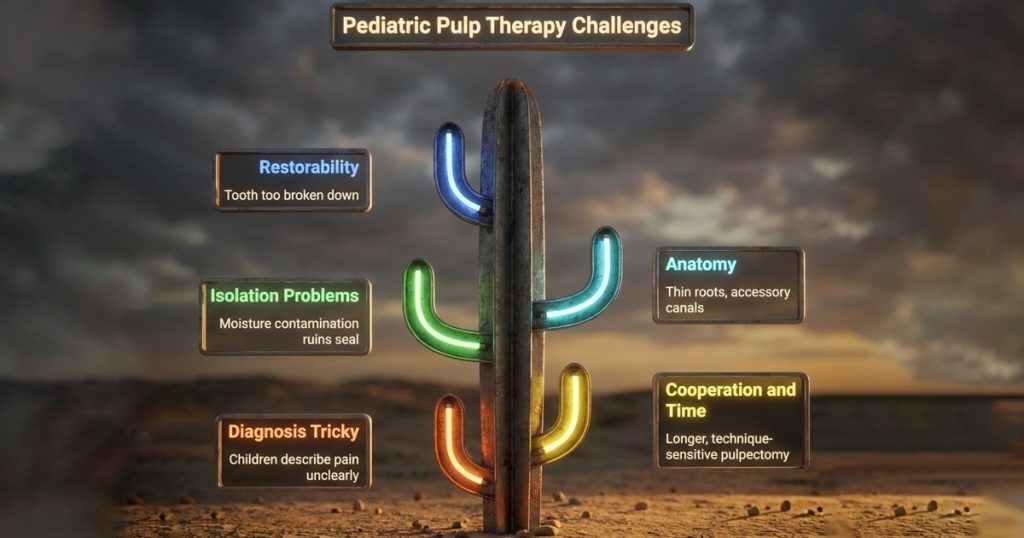
- Diagnosis is tricky
- Children may not describe pain clearly
- Primary teeth don’t always show classic periapical patterns (furcation is common)
- Cooperation and time
- Pulpectomy is longer and technique-sensitive
- Limited attention span affects outcome
- Isolation problems
- Moisture contamination ruins seal and increases failure risk
- Anatomy
- Thin roots, accessory canals, ongoing physiologic resorption
- Restorability
- Pulp therapy fails quickly if the tooth is too broken down or the final seal is weak
Recent Advances (What’s changing in clinics)
A few trends are shaping current paediatric pulp therapy:
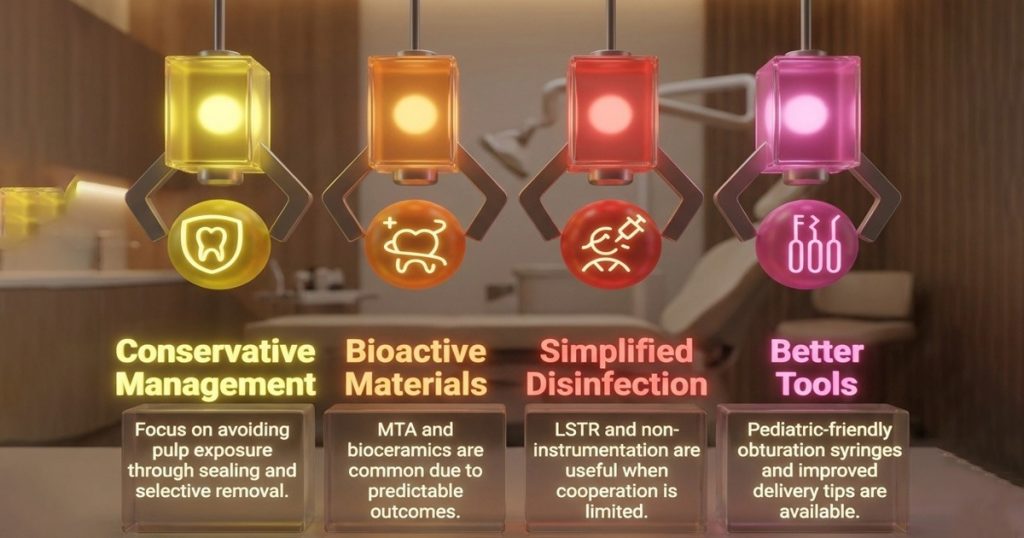
- Shift toward conservative caries management
- More focus on avoiding pulp exposure when possible (good sealing strategies, selective caries removal)
- Bioactive materials becoming routine
- MTA/Biodentine and similar bioceramics are more common due to predictable outcomes
- Simplified disinfection options for difficult cases
- LSTR / Non-instrumentation endodontic treatment (case-dependent)
- Useful when child cooperation is limited and the tooth is close to exfoliation
- Not a universal replacement, but a practical tool in selected cases
- Better tools
- Pediatric-friendly obturation syringes and improved delivery tips
- Rotary options exist but must be used carefully in primary canals
Conclusion
Paediatric pulp therapy works best when diagnosis, isolation, and the final seal are done properly. For vital cases, pulpotomy with bioactive materials like MTA or Bio dentine gives predictable outcomes when followed by full coverage restoration. For non-vital teeth, a well-cleaned pulpectomy with a resorbable obturating paste and a tight coronal seal helps the tooth stay functional until exfoliation. When restorability or cooperation is poor, choosing extraction or simplified protocols early can save chair time and prevent repeat infection.
FAQs
Always judge the radicular pulp response. If bleeding is bright red and easily controlled, pulpotomy is appropriate. Uncontrolled bleeding, suppuration, or a furcation radiolucency usually indicates pulpectomy or extraction.
While not legally mandatory, a stainless steel crown significantly improves success rates. Simple intracoronal restorations often fail due to microleakage, leading to early pulpotomy failure.
Yes. Both materials can be placed directly over the pulp stumps. After setting, they should be covered with a suitable base before final restoration to ensure a durable coronal seal.
Clinically, absence of pain, swelling, or mobility is a good sign within weeks. Radiographic evaluation at 6–12 months is important to confirm absence of furcation pathology or internal resorption.
The most common cause is poor coronal seal, not the medicament itself. Inadequate isolation, marginal leakage, or delayed full coverage restoration often lead to failure.




No Comment