Crestal vs. Lateral Sinus Lift: When to Use Which Technique?
Introduction
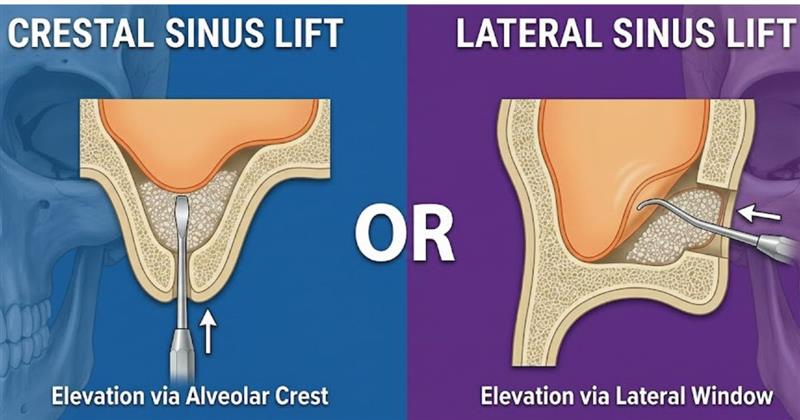
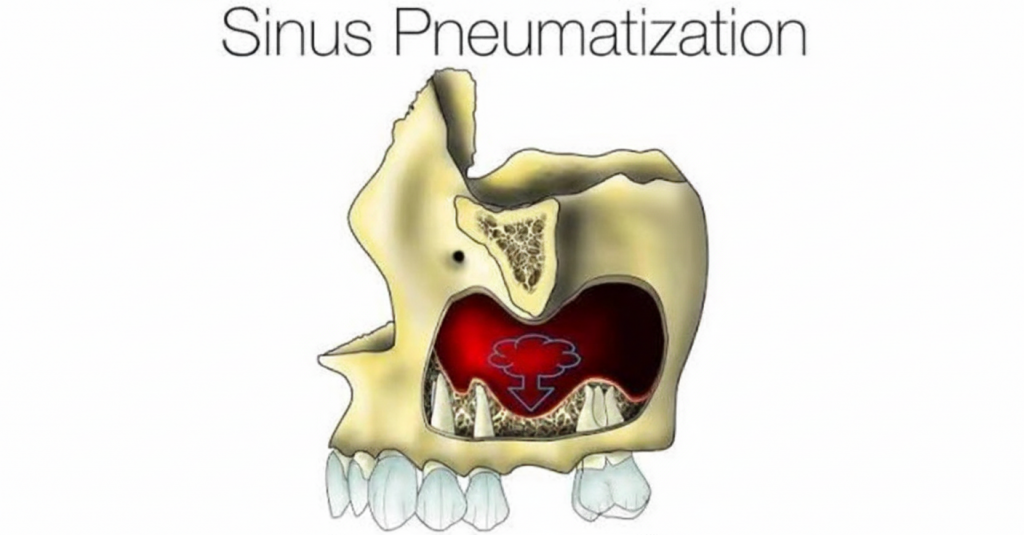
Loss of maxillary premolars and molars often leads to pneumatization of the sinus and resorption of the alveolar ridge. When implant therapy is planned in these sites, the surgeon must decide how to increase the available bone height safely and predictably. Two broad approaches are used to elevate the sinus floor: the lateral (open) sinus lift and the crestal (transcrestal) sinus lift. Each technique has advantages, limitations and contemporary refinements.

Significance of Sinus Lift Surgery
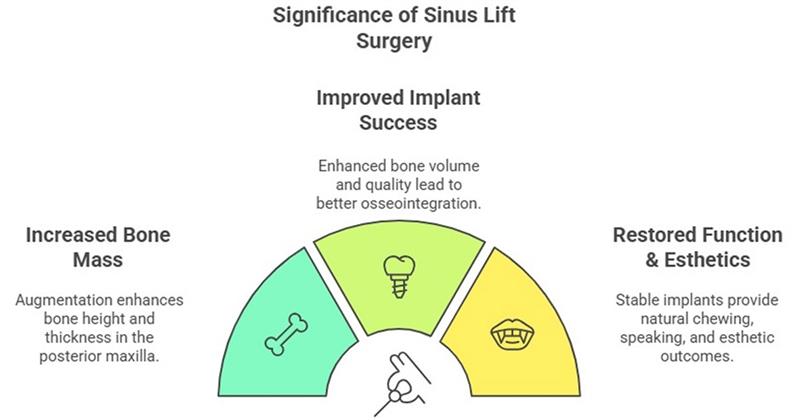
Sinus lift surgery is therefore not merely a technical exercise but a foundational step for predictable implant therapy in the atrophic posterior maxilla. Comprehensive presurgical assessment and selection of the appropriate technique are essential to minimize complications.
Product: Waldent Advance Sinus Elevation Kit 14-Pcs Set
Classification by Residual Bone Height

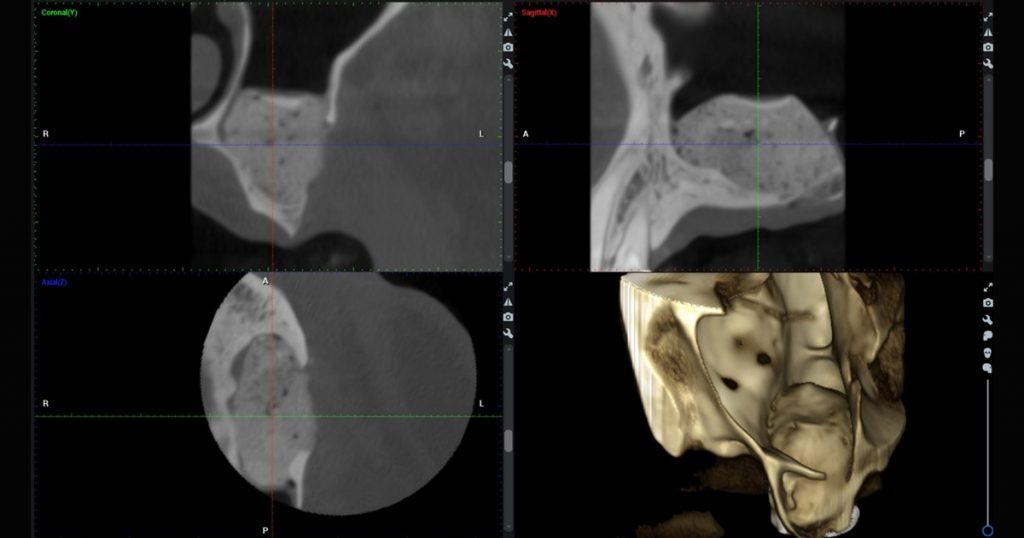
Treatment planning begins with conebeam computed tomography (CBCT) to measure residual bone height (RBH) and evaluate sinus anatomy. A commonly used classification divides cases into three groups:
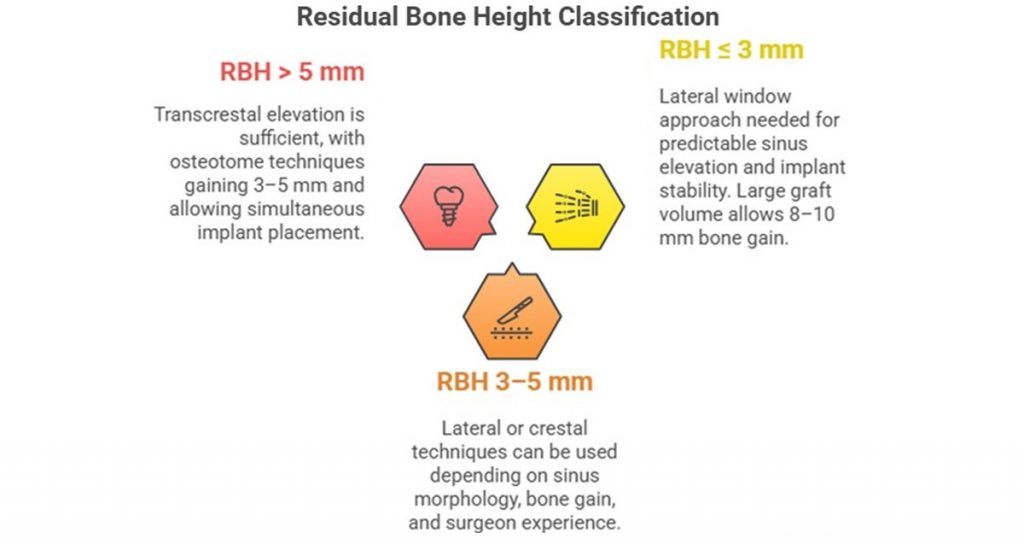
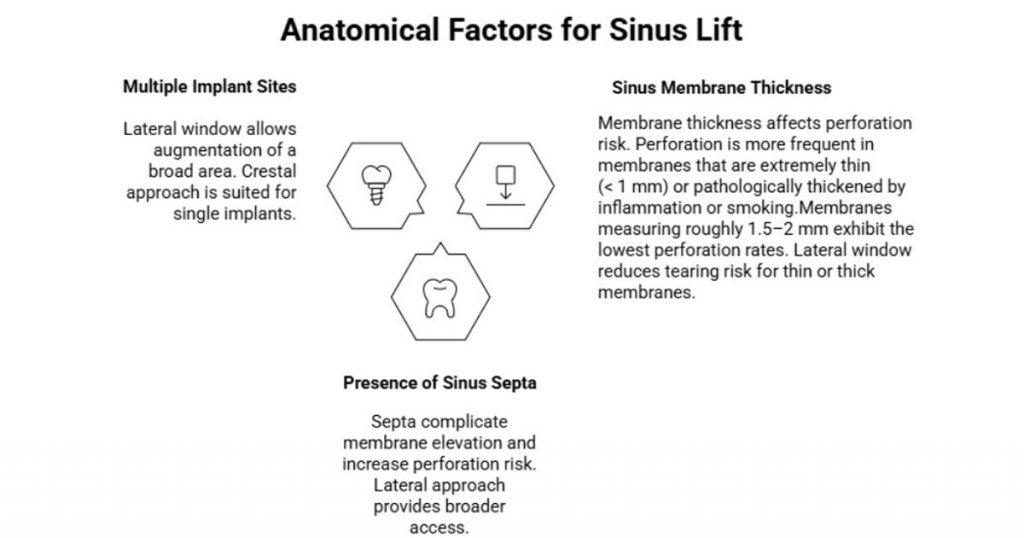
Residual bone height is not the only factor. Sinus membrane thickness, presence of septa, and access to multiple implant sites also influence technique selection.
Anatomical factors for Sinus Lift
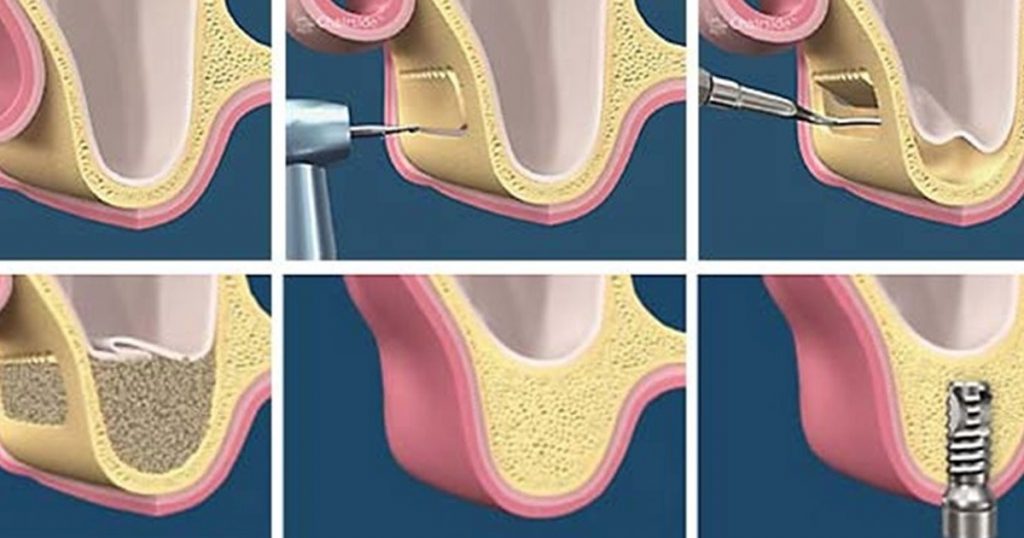
Lateral Sinus Lift
The lateral (open) approach involves creating an access window in the lateral sinus wall, gently elevating the Schneiderian membrane and placing bone graft material. Despite the trend toward minimally invasive procedures, the lateral technique remains relevant because it:
- Provides direct access to overcome obstacles such as sinus septa and thick membranes
- Allows augmentation irrespective of RBH, making it the technique of choice when only 1–3 mm of bone remain
- Facilitates multiple implant sites through a single window
- Permits management of complications such as membrane perforation under direct vision
Lateral sinus lifts are more invasive than transcrestal methods and require a larger flap and osteotomy. However, refinements such as smaller windows and the use of piezoelectric devices have reduced morbidity and improved precision. Modern piezoelectric units cut bone with ultrasonic vibrations while sparing soft tissues, lowering the risk of membrane perforation and shortening operative time.
Product: Julldent Lateral Sinus Window Bur
Innovations in Lateral Sinus Elevation:
Piezoelectric and Ultrasonic Systems
- Ultrasonic vibration selectively cuts mineralized tissue
- Preserves soft tissue integrity, including sinus membrane
- Enables precise lateral window preparation
- Reduces risk of membrane perforation
- Minimizes heat generation and surgical trauma

Product: Woodpecker Surgic Touch Piezosurgery Unit
Minimally Invasive Lateral Window Design
- Smaller, strategically positioned lateral windows
- Reduced flap reflection and surgical morbidity
- Maintains adequate access for membrane elevation and graft placement
- Results in less postoperative pain and swelling
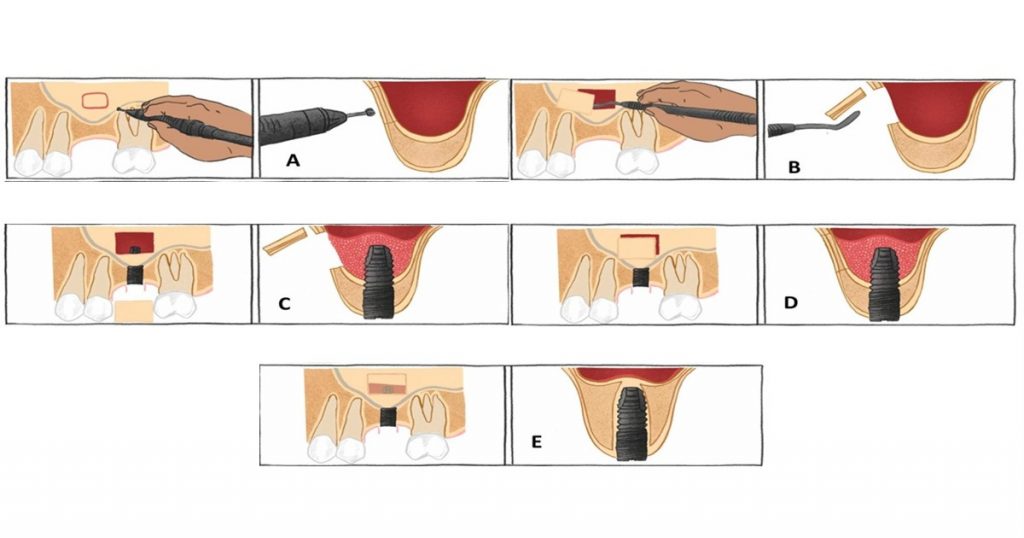
Digitally Planned Lateral Sinus Lifts
- CBCT-based virtual planning of window location and size
- 3D-printed surgical guides enhance accuracy
- Improves consistency and reproducibility
- Shortens operative time
- Reduces intra-operative uncertainty
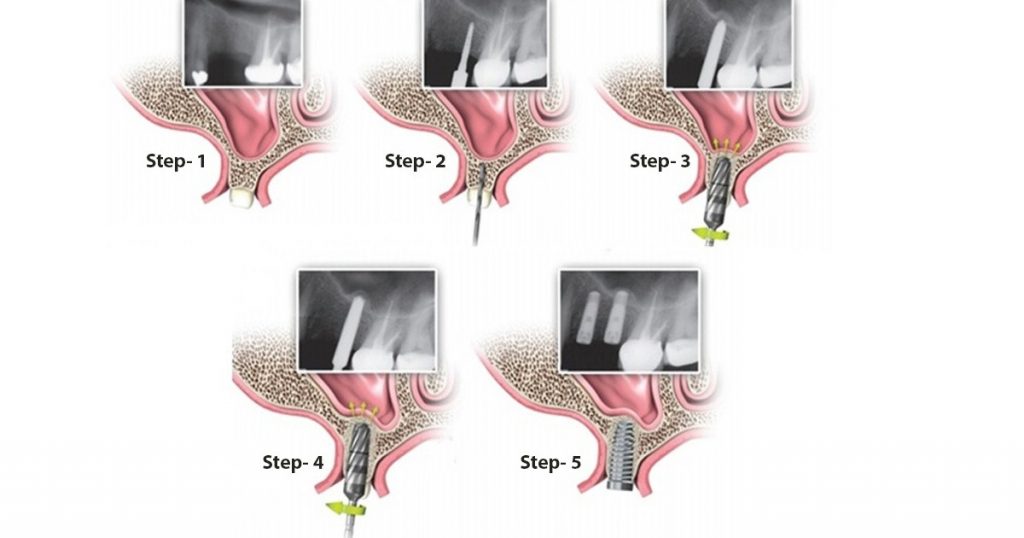
Crestal Sinus Lift
The crestal (transcrestal) approach was introduced by Summers as a less invasive alternative. Through the implant osteotomy, the sinus floor is fractured with osteotomes or specialized drills and the membrane is lifted. Traditionally the technique was reserved for sites with at least 5 mm of bone, but contemporary tools have expanded its indications:
- Sites with moderate bone (≥5 mm): Conventional osteotome methods can safely gain 3–4 mm of bone and allow simultaneous implant placement
- Sites with 3–5 mm of bone: Crestal lifts combined with tapered implants and bone grafting kits can achieve adequate stability
- Sites with <3 mm: Recent case reports demonstrate successful transcrestal augmentation below 3 mm using hydraulic pressure and rounded drills, provided that careful technique and implant design are used.
The crestal approach minimizes surgical trauma and postoperative discomfort, but it offers limited visibility and carries a risk of membrane perforation. Innovations described below mitigate these limitations and have increased the predictability of transcrestal lifts.
Product: Julldent Crestal Approach Sinus Cas-kit
Innovations in Crestal Sinus Elevation:
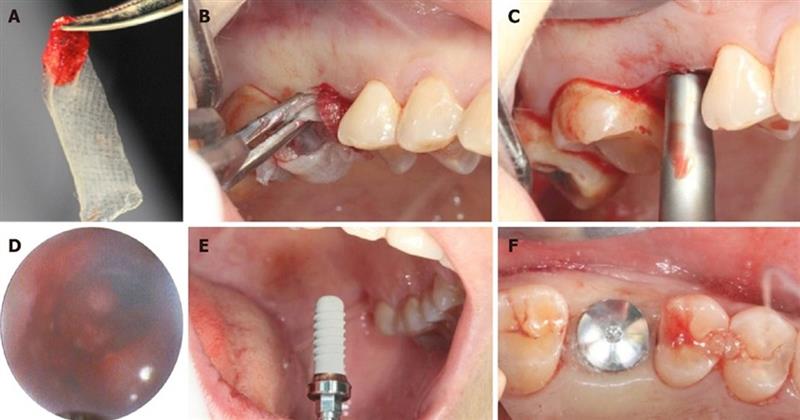
Endoscopic-Assisted Crestal Lift
- Rigid endoscope introduced through the osteotomy
- Enables real-time visualization of the Schneiderian membrane
- Significantly reduces membrane perforation risk
- Allows early detection of micro-perforations
- Supports intra-operative decision-making (continue vs abort)
- Improves postoperative bone density outcomes
- Requires additional equipment and slightly longer operative time
Hydraulic Sinus Elevation Techniques
- Uses controlled hydraulic pressure to detach the sinus membrane
- Saline delivered incrementally through depth-controlled osteotomy drills
- Provides uniform membrane elevation with minimal mechanical trauma
- Enhances safety in sites with limited residual bone height
- Improves predictability compared to conventional osteotomes


Product: Julldent Aqua Sinus Tip /Hydraulic Tip
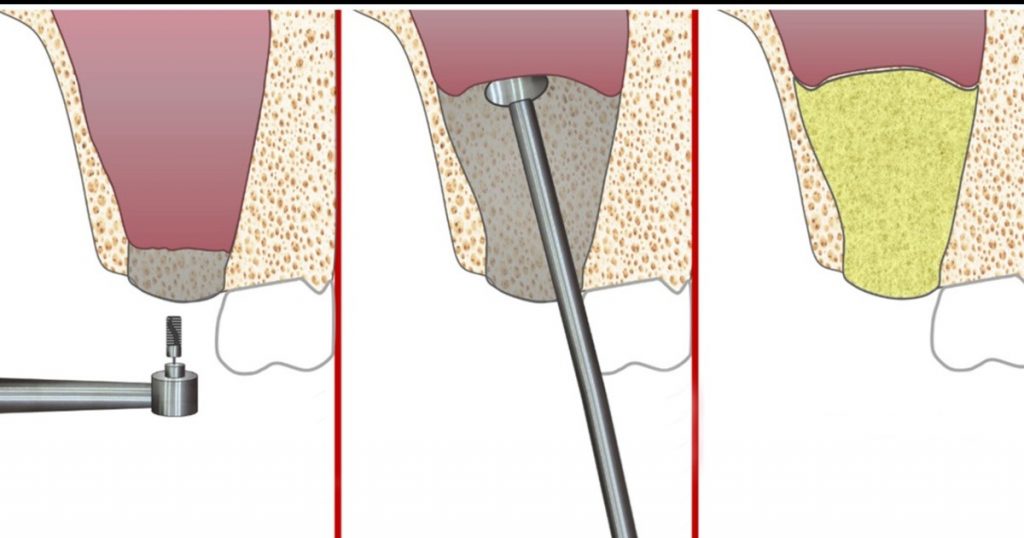
Antral Membrane Balloon Elevation (AMBE)
- Inflatable balloon inserted through the crestal access
- Gradual, controlled elevation of the sinus membrane
- Lower membrane perforation rates compared to malleting techniques
- Allows greater vertical bone gain in a minimally invasive manner
- Particularly useful for single-implant sites
Osseodensification (Densifying Burs)
- Reverse-rotating burs compact bone instead of removing it
- Simultaneously elevate sinus floor and increase peri-implant bone density
- Improves primary implant stability
- Harvests autogenous bone chips during site preparation
- Reduces dependency on additional graft material
Biologics and Growth Factors
- Platelet-rich fibrin (PRF) enhances angiogenesis and healing
- Improves graft stability when combined with xenografts
- Recombinant BMPs stimulate osteogenesis
- May eliminate need for autogenous bone harvesting
- Improves predictability of crestal and lateral sinus augmentation
DecisionMaking: Selecting the Appropriate Technique
The choice between a crestal and a lateral sinus lift should be individualized. The following table summarizes key factors and the preferred technique under typical conditions. These guidelines serve as a starting point; clinician judgment and patientspecific considerations remain paramount.
| Factor | Lateral Window (Open) | Crestal (Transcrestal) |
|---|---|---|
| Residual bone height | Recommended when <3 mm of bone remains; direct access allows augmentation irrespective of RBH | Suitable when ≥5 mm is available; recent innovations extend use to 3–5 mm and select cases below 3 mm |
| Required bone gain | Gains 8–10 mm of vertical height; preferred for large augmentations or multiple implants | Typically achieves 3–5 mm; adequate for single implants requiring modest elevation |
| Sinus anatomy and pathology | Ideal when sinus has septa, mucosal thickening or cysts; direct visualization facilitates management | Best for simple domeshaped sinuses without pathology; limited visibility makes handling septa challenging |
| Expertise and equipment | Requires proficiency in flap design, window creation and membrane management; piezoelectric tools and digital guides improve outcomes | Newer techniques (endoscopy, hydraulic lifts, osseodensification) demand specialized training and instruments |
| Intraoperative flexibility | Direct visualization enables repair of perforations or management of unexpected pathology | Limited visibility; minor perforations may go undetected without endoscopic assistance |
Clinicians should also consider patient preferences, cost, surgical time and recovery expectations when selecting the technique.
Conclusion
Both crestal and lateral sinus lifts play essential roles in the rehabilitation of the posterior maxilla. The lateral approach remains the gold standard for cases with severe bone deficiency or complex sinus anatomy because it offers maximum visibility and bone gain. The crestal approach, once limited to moderate bone heights, has benefited from innovations such as endoscopic guidance, hydraulic and balloon systems, osseodensification and biologic enhancers. These developments expand its indications and reduce patient morbidity. Ultimately, proper case assessment, a thorough understanding of the available techniques and careful execution are key to successful sinus augmentation.
FAQ’s
A lateral sinus lift is preferred when residual bone height is <3 mm, when significant vertical bone gain is required, or when sinus anatomy is complex (presence of septa, thick membrane, or pathology), as it allows direct visualization and better control.
Yes. Simultaneous implant placement is commonly performed when adequate primary stability can be achieved—typically in crestal lifts with sufficient residual bone and in selected lateral lift cases. Otherwise, a staged approach is advised.
The most frequent complication is Schneiderian membrane perforation. Others include sinusitis, graft migration, infection, and postoperative swelling. The risk is reduced with proper case selection, gentle technique, and use of piezoelectric or minimally invasive tools.
Technologies such as piezoelectric surgery, endoscopic assistance, hydraulic elevation, balloon systems, and osseodensification reduce mechanical trauma, improve membrane control, enhance primary stability, and increase overall predictability of both crestal and lateral approaches.
The decision should be based on residual bone height, required bone gain, sinus anatomy, number of implants planned, clinician experience, and available equipment, along with patient-specific factors such as healing capacity and treatment expectations.




No Comment