Bone Grafts and Membranes: Everything Dentists Need to Know

In the field of periodontics and implantology, achieving optimal bone regeneration is essential for long-term success. Whether dealing with bone loss due to periodontal disease, trauma, or tooth extraction, the use of bone grafts and membranes has become a cornerstone in modern dental practice. These materials support bone regeneration, improve surgical outcomes, and help maintain structural integrity for implant placement or periodontal repair.
In this blog, we’ll quickly revisit what bone grafts and membranes are, explore their types, and understand how they can be collected.
What are Bone Grafts and Membranes?
A bone graft is bone taken from the patient themself, a donor (which can be either human or animal), or formed from a synthetic material. This graft can either replace the missing bone altogether or act as a scaffolding on which the patient’s own bone can grow.
Bone membranes are resorbable or non-resorbable materials that serve as a protective barrier to prevent unwanted tissue from growing into the surgical area, allowing the bone to regenerate.
Classification of Bone Grafts:
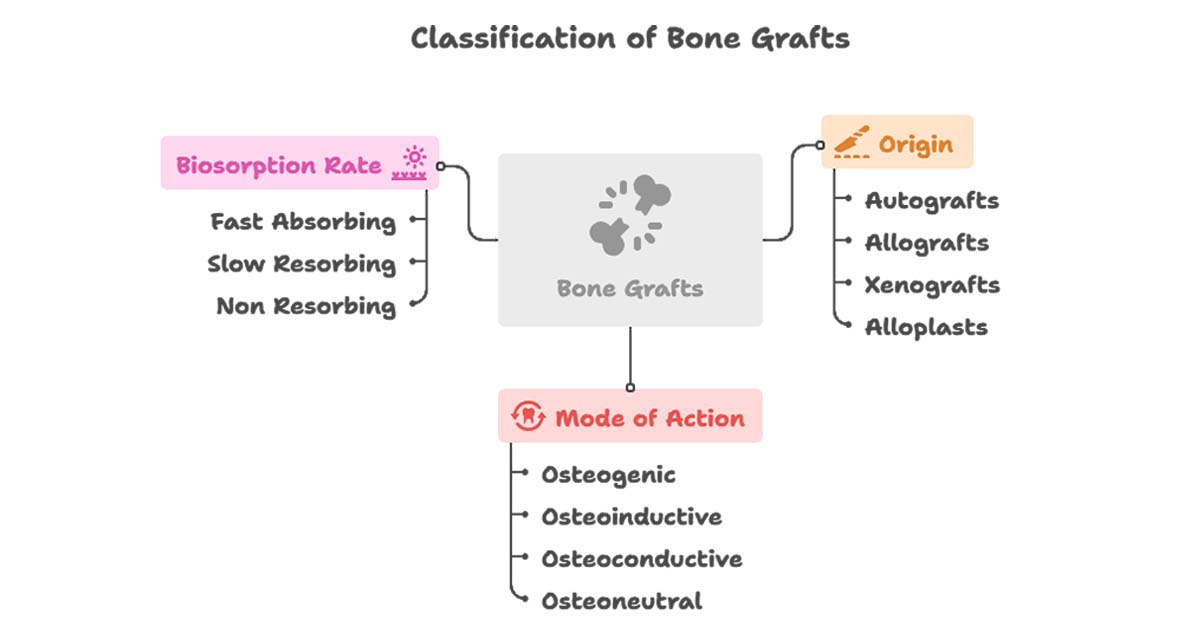
Bone Grafts based on Origin:
1. Autografts: Where the bone is obtained from the same individual.
2. Allografts: Obtained from different individuals of the same species.
3. Xenografts: Bone obtained from a different species, usually of bovine or porcine origin.
4. Alloplasts: Synthetic graft materials or bone substitutes.
Bone Grafts based on Mode of their Action as under:
- Osteogenic grafts where the grafted tissue contains the cells necessary to form new bone. Only autografts have this capacity and hence are considered as gold standards.
- Osteoinductive grafts which have the capacity to convert the surrounding tissue to form osteoblasts through the release of bone morphogenic proteins.
- Osteoconductive which is a physical effect by which the matrix of the graft forms a scaffold that favors outside cells and blood vessels to penetrate graft and form new bone.
- Osteoneutral graft is that which merely fills the bone defect without producing any effect and often gets encapsulated.
Bone Grafts depending on the Rate of their Biosorption:
- Fast Absorbing where in the graft gets resorbed within 8 to 10 weeks after placement.
- Slow resorbing in which case the grafted material stays for many months.
- Non resorbing ones are those which do not resorb for years
Properties of an Ideal Bone Graft Material:
- Non -toxic
- Non-antigenic
- Resistant to infection
- Predictability
- Clinical feasibility
- Easy adaptability
- Readily and sufficiently available.
- Minimal operative and post operative hazards.
- Adequate bone fill and promotion of new attachment including cementogenesis.
- Cost-effective and acceptable to the patient.

Types of Bone Grafts:
1. Autogenous Bone Grafts-
a. Bone from intraoral sites:
Bone grafts for the reconstruction of bone defects produced by periodontal diseases can be taken from intraoral sites like healing extraction wounds, bone from edentulous ridges, bone trephined from within the jaw without damaging the roots, newly formed bone in wounds especially created for the purpose, bone removed from the tuberosity or the ramus, bone removed during osteoplasty and ostectomy, and the lingual surface of the mandible or maxilla at least 5 mm from the roots.
One technique of collecting autogenous bone grafts is “Osseous Coagulum.” In this, small particles are ground from the cortical bone. Bone is removed with a carbide bur and placed in a sterile dappen dish and used to fill the defect.
The particles help provide additional surface area for the interaction of the cellular and vascular elements. Another advantage is that it is obtained from an already exposed area during surgery.
The disadvantage is relatively low predictability and the inability to procure adequate material for large defects. Also, aspiration cannot be done to accumulate the coagulum.
The “Bone Blend” technique overcomes the disadvantages of the Osseous Coagulum technique. This technique uses an autoclaved plastic capsule and pestle. Bone is removed from a predetermined site, triturated in the capsule to a workable, plastic-like mass, and packed into bony defects. This way, one knows the amount collected beforehand for a defect.
b. Cancellous Bone Marrow Transplants:
Cancellous bone can be obtained from the maxillary tuberosity, edentulous areas, and healing sockets. A ridge incision is made distally from the last molar, and bone is removed with a curved rongeur. It is important to ensure that the incision is not extended too far distally to avoid entering the mucosal tissue of the pharyngeal area, and areas are radiographed before starting the procedure to plan accordingly.
Extraction sockets are allowed to heal for 8–12 weeks before re-entering and removing the newly formed bone from the apical portion, which is used as the donor material.
c. Bone Swaging:
The bone swaging technique requires an edentulous area adjacent to the defect, from which the bone is pushed into contact with the root surface without fracturing the bone at its base. One disadvantage is that it is technically difficult, and its usefulness is limited.
d. Bone from Extraoral Sites:
The use of fresh or preserved iliac cancellous marrow and bone from the tibia has been extensively investigated. It has also been successful in furcations and even supracrestally to some extent. However, there were a number of postoperative problems such as infection, bone exfoliation, sequestration, varying rates of healing, root resorption, and rapid recurrence of the defect. These only increased the patient’s expense and the difficulty in procuring the donor material.
2. Bone Allografts
These are commercially available from tissue banks. They are obtained from cortical bone within 12 hours of the donor’s death, defatted, cut into pieces, washed in absolute alcohol, and deep-frozen. The material may be demineralised and subsequently ground and sieved to a particle size of 250–750 µm, and then freeze-dried. Finally, it is vacuum-sealed in glass vials.
A number of steps are taken to eliminate any viral infectivity. Various tests are done on cadaver tissues to exclude individuals with any infection or malignant disease. The tissue obtained is also treated with chemical agents and acids to inactivate any viruses still present.
Freeze-Dried Bone Allograft (FDBA) is one of the types of bone allografts, wherein the FDBA is osteoconductive, and demineralised FDBA (another type of allograft) is an osteoinductive graft. It is also found in studies that DFDBA has higher osteogenic potential than FDBA.
3. Xenografts:
Bone products from other species are called xenografts. Most of the xenografts are no longer in use after various trials.
Currently, an anorganic, bovine-derived bone marketed under the brand name Bio-Oss (Osteohealth) has been used for a few procedures like periodontal defects or implant surgeries. It is an osteoconductive, porous bone mineral matrix derived from bovine cancellous or cortical bone. The organic components of the bone are removed, but the trabecular architecture and porosity are retained.
These physical features permit clot stabilization and revascularization, allowing for the migration of osteoblasts, leading to osteogenesis. Bio-Oss is biocompatible with the adjacent tissues, eliciting no systemic immune response.
4. Alloplasts (Synthetic Bone Graft Materials):
The risk of disease transmission and religious constraints led researchers to look for synthetic bone replacement grafts.
Following are some materials that came and went without any remarkable history in bone grafting, such as calcium phosphate biomaterials, bioactive glass, coral-activated materials, etc. These could not be used either because of their encapsulation in collagen or their slow or absent resorption, leading to their discontinuation.
Types of Bone Membranes:
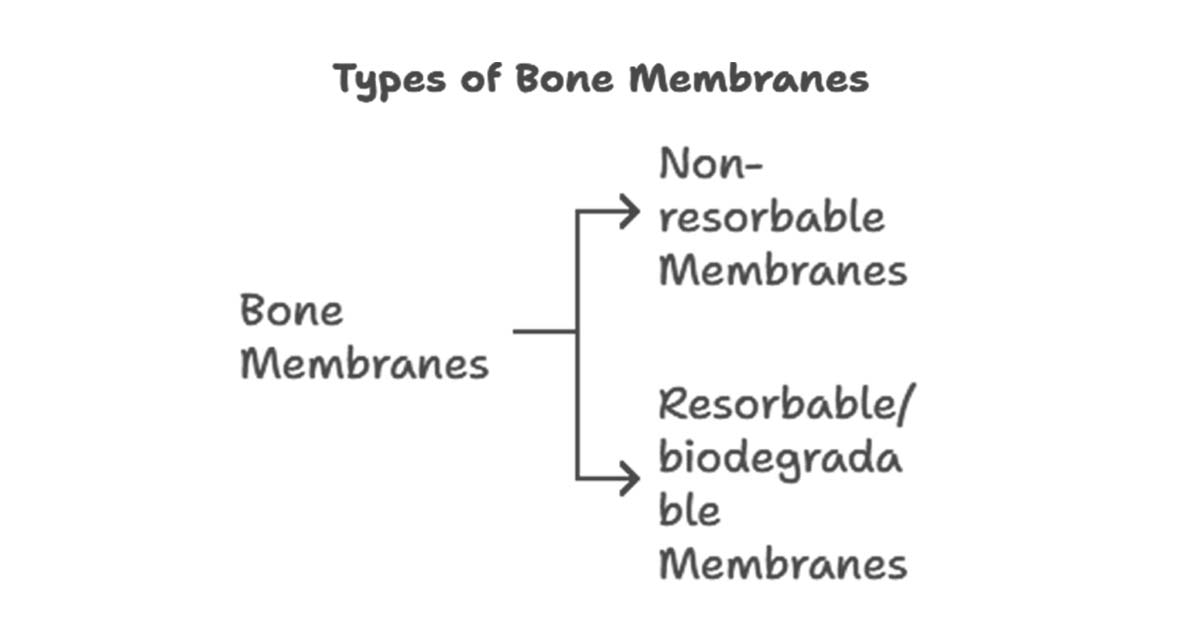
1. Non-resorbable membranes
These membranes are non-resorbable and need to be removed after an appropriate amount of time. Non-resorbable membranes are made up of synthetic materials like expanded polytetrafluoroethylene (ePTFE). They are biocompatible, act as a cellular barrier, provide space for the healing tissue, and are clinically manageable.
These are also available as titanium-reinforced ePTFE, which includes a mouldable titanium layer to provide rigidity, shape the graft, and thus permit correction of larger defects.
One major problem faced with the usage of these membranes is that the membrane can become exposed to the oral environment during healing. Upon exposure, the membrane is contaminated and colonized by oral microflora. Several studies have shown that contamination of the surgical site can lead to decreased formation of new attachment.
Read Also: Mastering Suturing Techniques and Choosing the Right Materials in Dentistry
2. Resorbable/biodegradable membranes
The resorbable membranes have majorly replaced the routine use of ePTFE membranes in periodontal procedure along with others. There are basically three types of bioresorbable membranes: a. Polyglycoside synthetic polymers; b. Collagen; c. calcium sulfate.
These membranes are more tissue compatible, timing of resorption can easily be regulated, and another surgical procedure is not required to retrieve the non-resorbed membrane.
Conclusion:
Bone grafts and membranes play a vital role in enhancing the success of periodontal and implant procedures by supporting bone regeneration and maintaining structural integrity. Understanding the different types, their biological behavior, and methods of application allows clinicians to choose the most appropriate material for each clinical scenario.
At Dentalkart, we offer a wide range of bone graft materials and membranes, carefully selected for dental professionals. Explore our collection to find high-quality products that meet your clinical needs — all in one place at Dentalkart.




No Comment