Lithium Disilicate vs Zirconia Crowns: Clinical Comparison Guide
Introduction
Selecting the right crown material has become more important than ever in modern restorative dentistry. Patients today expect restorations that not only last long but also look natural and feel comfortable. With advancements in ceramic materials, dentists now have excellent options, but this also means more decision-making at the chairside.
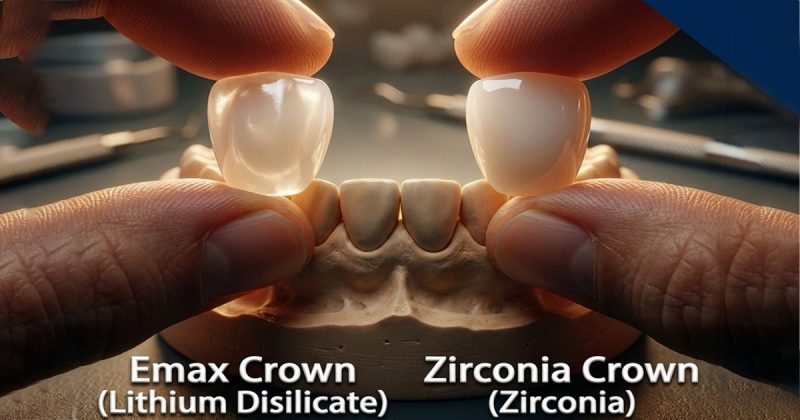
Among all-ceramic restorations, lithium disilicate and zirconia stand out as the most commonly used materials in 2026. Both are reliable, clinically proven, and widely accepted. However, they differ significantly in terms of strength, aesthetics, preparation requirements, and indications. Understanding these differences helps dentists make confident, case-specific choices.
This blog offers a clear comparison of lithium disilicate and zirconia crowns, including clinical indications, advantages, limitations, and a quick-reference comparison table.
Understanding the Two Materials
What Is Lithium Disilicate?
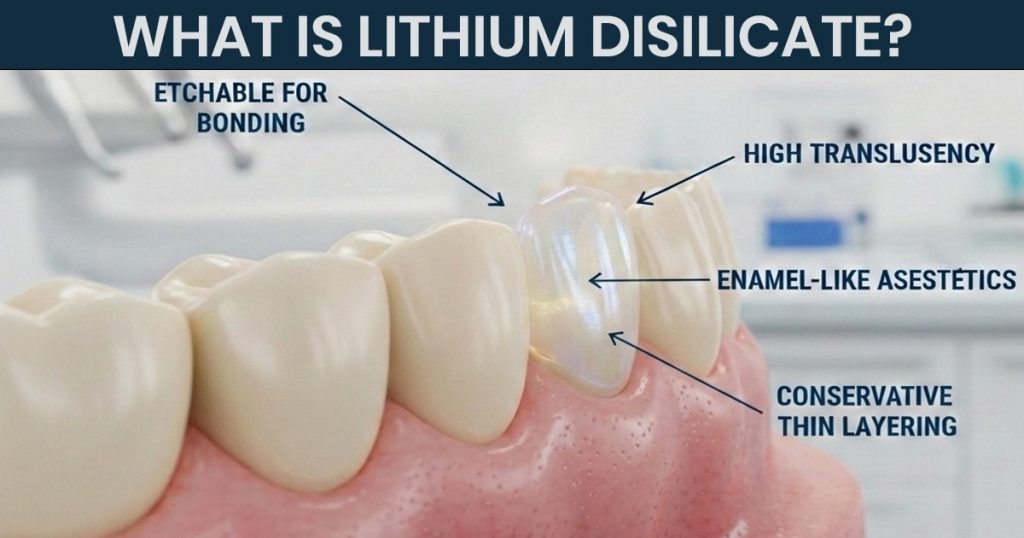
Lithium disilicate is a glass-ceramic material valued for its excellent aesthetics and enamel-like translucency. It blends well with natural dentition and is widely used in visible areas of the mouth.
Key features include:
- High translucency and natural appearance
- Excellent shade matching
- Etchable surface for strong bonding
- Suitable for conservative restorations
What Is Zirconia?
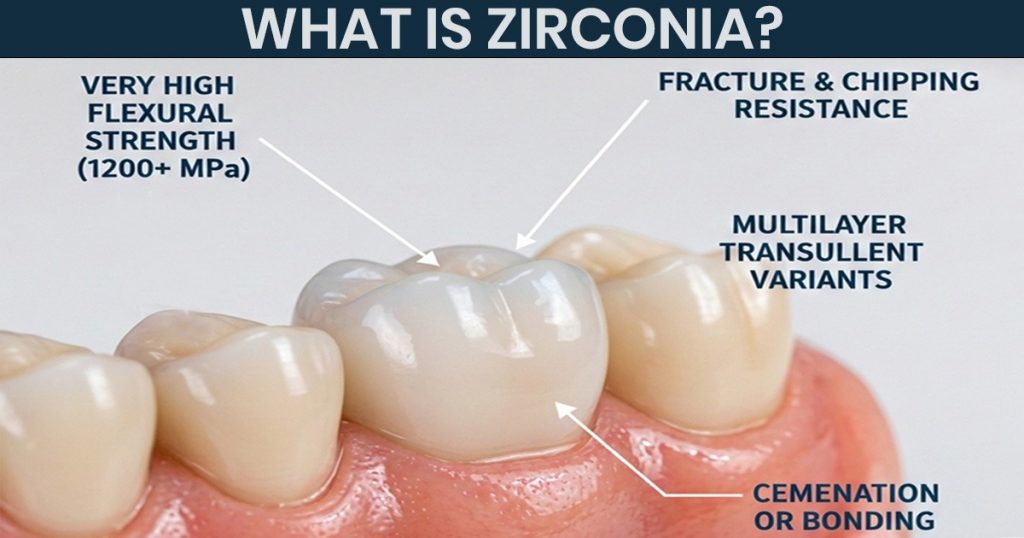
Zirconia is a polycrystalline ceramic known for its exceptional strength and fracture resistance. It has become the material of choice for restorations exposed to high occlusal forces.
Key features include:
- Very high flexural strength
- High resistance to fracture and chipping
- Available in multilayer and translucent variants
- Suitable for cementation or bonding
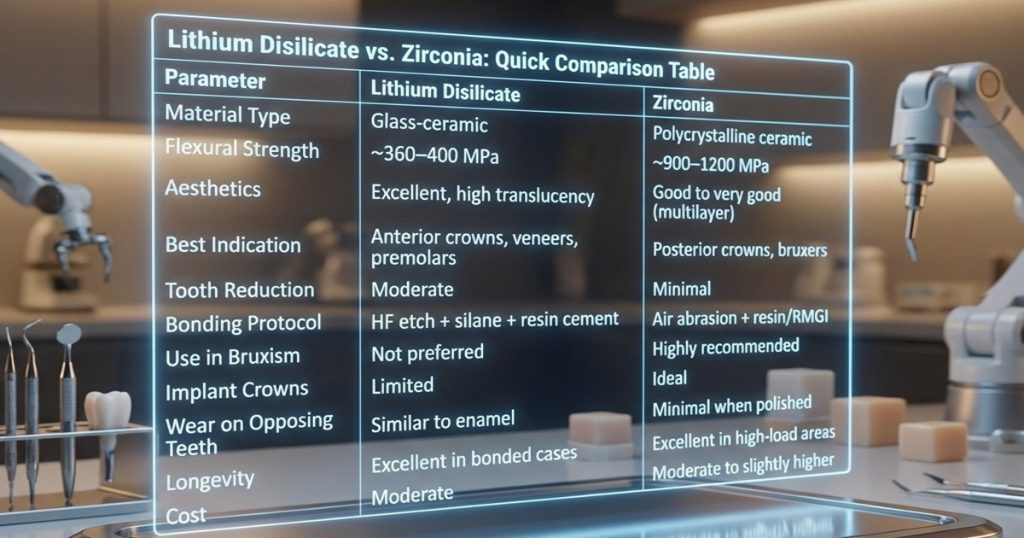
Strength and Load-Bearing Capacity
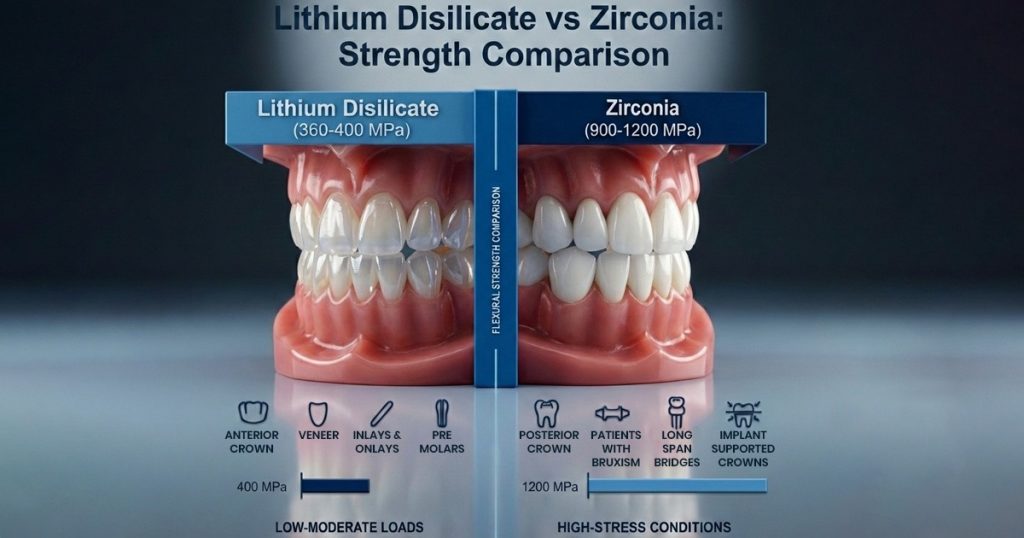
Lithium Disilicate
- Flexural strength of approximately 360–400 MPa
- Suitable for:
- Anterior crowns
- Premolars
- Veneers
- Inlays and onlays
It performs well under low to moderate occlusal loads but is not ideal for heavy posterior forces.
Zirconia
- Flexural strength of approximately 900–1200 MPa
- Suitable for:
- Posterior crowns
- Patients with bruxism
- Long-span bridges
- Implant-supported crowns
Zirconia offers excellent durability even in high-stress conditions.
Aesthetic Outcomes

Lithium Disilicate
Lithium disilicate remains the preferred option when aesthetics are critical.
Advantages:
- Superior translucency
- Natural light transmission
- Excellent for smile zone restorations
Limitations:
- Lower masking ability in discolored teeth
Zirconia
Modern zirconia materials have improved aesthetics compared to earlier generations.
Advantages:
- Multilayer zirconia improves shade transition
- Acceptable aesthetics in posterior and selected anterior cases
Limitations:
- Still less translucent than lithium disilicate in highly aesthetic cases
Tooth Preparation and Conservation
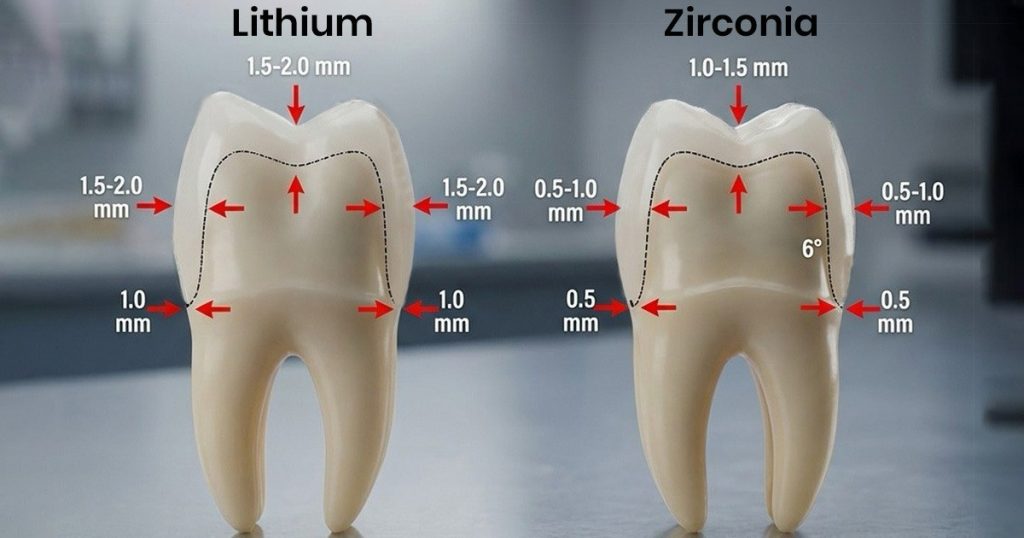
Lithium Disilicate
- Requires slightly more tooth reduction
- Rounded internal line angles recommended
- Best results when adequate enamel is available for bonding
Zirconia
- Allows minimal tooth reduction
- Suitable for teeth with compromised structure
- Maintains strength even at reduced thickness
Cementation and Bonding Protocols
Lithium Disilicate

- Etched with hydrofluoric acid
- Requires silane application
- Adhesively bonded using resin cement
This bonding process enhances strength and retention.
Zirconia

- Not etchable with HF acid
- Requires air abrasion
- Cemented using resin-modified or resin cement
Bonding is simpler but technique-sensitive.
Lithium Disilicate vs. Zirconia: Quick Comparison Table
How Occlusion and Patient Habits Influence Material Choice
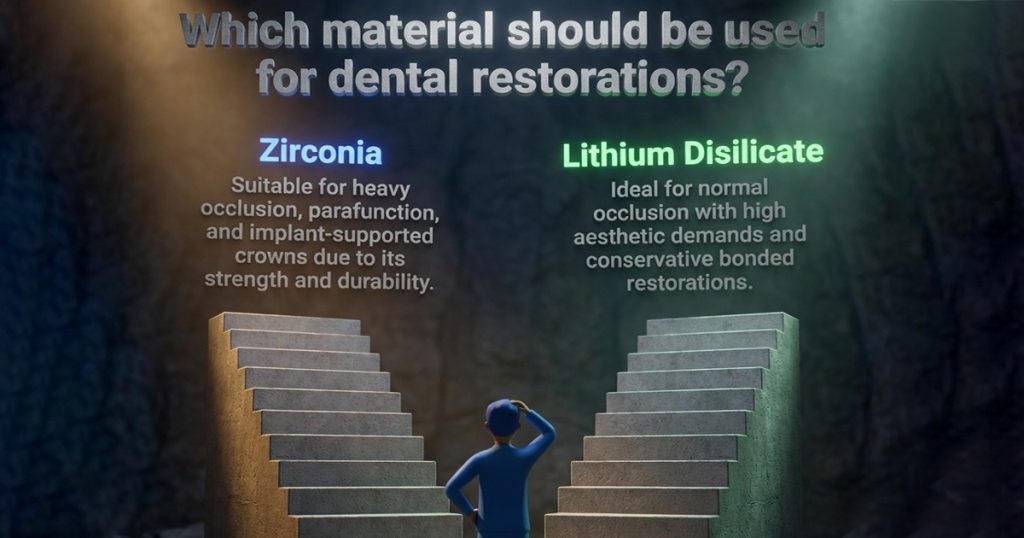
Material selection should never be based on strength or aesthetics alone. Occlusion and patient habits play a major role in long-term success.
Dentists should assess:
- Presence of bruxism or clenching
- Opposing dentition (natural teeth vs restorations)
- Occlusal scheme and guidance
- Parafunctional habits
Clinical guidance:
- Heavy occlusion or parafunction → Zirconia
- Normal occlusion with high aesthetic demand → Lithium disilicate
- Implant-supported crowns → Zirconia
- Conservative bonded restorations → Lithium disilicate
Matching material choice to occlusal risk reduces failures significantly.
Wear on Opposing Dentition
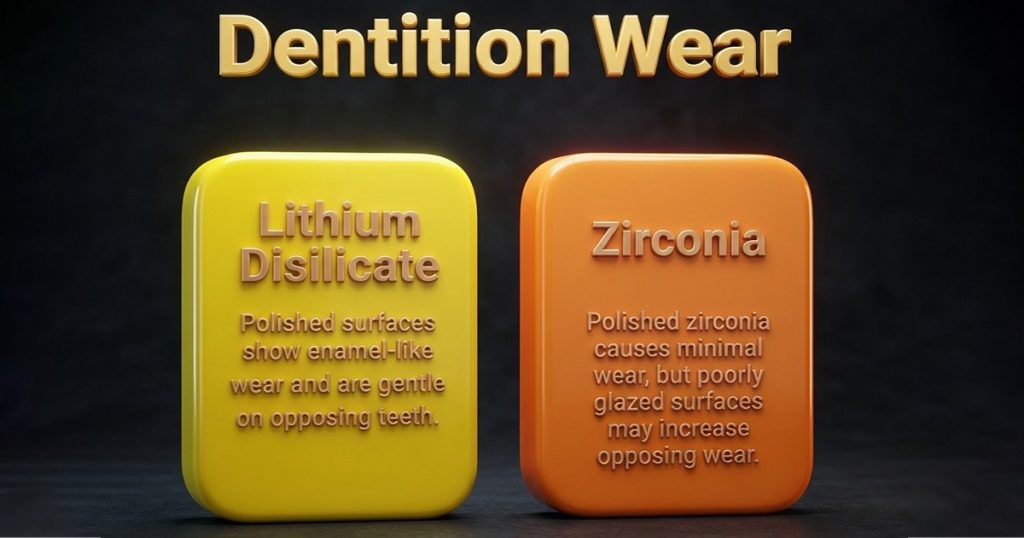
Lithium Disilicate
- Polished surfaces show enamel-like wear
- Gentle on opposing teeth
Zirconia
- Polished zirconia causes minimal wear
- Poorly glazed surfaces may increase opposing wear
Proper finishing and polishing are essential for both materials.
Longevity and Clinical Performance
Both materials demonstrate excellent long-term outcomes when used correctly.
- Lithium disilicate performs predictably in bonded, aesthetic cases
- Zirconia shows very low fracture rates in posterior and high-load situations
Correct case selection remains the key factor.
Common Clinical Mistakes to Avoid
- Using lithium disilicate in bruxism cases
- Choosing zirconia for highly aesthetic anterior restorations without proper shade planning
- Incorrect cementation protocols
- Inadequate polishing of zirconia surfaces
Avoiding these errors improves restoration longevity.
Final Thoughts
Lithium disilicate and zirconia are both excellent crown materials, each with clearly defined strengths. Lithium disilicate excels in aesthetics and bonded restorations, while zirconia offers unmatched strength and durability.
The best clinical outcomes are achieved when dentists select materials based on case requirements rather than routine preference. Understanding when and where to use each material allows dentists to deliver restorations that are functional, aesthetic, and long-lasting.
FAQ’s
Zirconia requires minimal tooth reduction and is ideal for teeth with compromised structure or limited interocclusal space.
Yes. Lithium disilicate requires adhesive bonding using HF etching, silane, and resin cement to achieve optimal strength and retention.
Zirconia is preferred for implant crowns due to its strength, durability, and resistance to fracture under occlusal load.
Yes, if proper adhesive bonding is done. Ensure sufficient enamel for reliable retention and avoid high occlusal stress.
Yes. Resin-modified or resin cements improve retention, especially when bonding is required for additional strength.




No Comment