Peri-Implantitis Management: Non-Surgical vs Surgical Approaches

Dental implants are now a routine part of everyday dental practice. From single-tooth replacements to full-mouth rehabilitations, implants have given dentists predictable, long-term solutions for missing teeth. However, with the rapid increase in implant placements, one complication is becoming more visible in clinics, i.e. peri-implantitis.
Peri-implantitis is no longer a rare complication. Many dentists encounter it during recall visits, routine cleanings, or when patients report discomfort around implants. The real question that most clinicians face is: Can this be managed non-surgically, or is surgery unavoidable?
This blog breaks down peri-implantitis management in a clear, practical way, comparing non-surgical and surgical approaches, so you can confidently choose the right treatment for your patient.
Understanding Peri-Implantitis
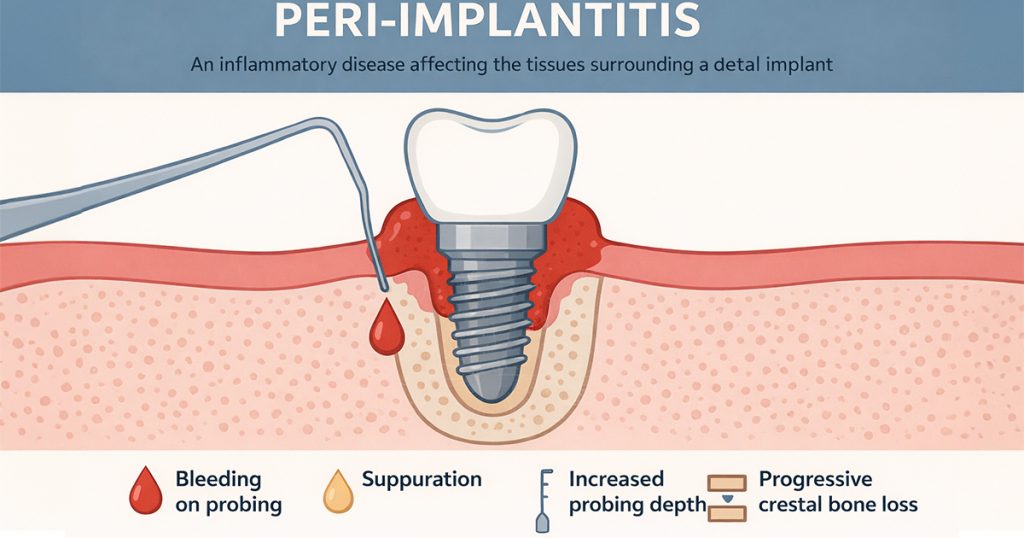
Peri-implantitis is an inflammatory disease affecting the tissues surrounding a dental implant.
Unlike peri-implant mucositis (which is reversible), peri-implantitis involves bone destruction, making timely intervention critical.
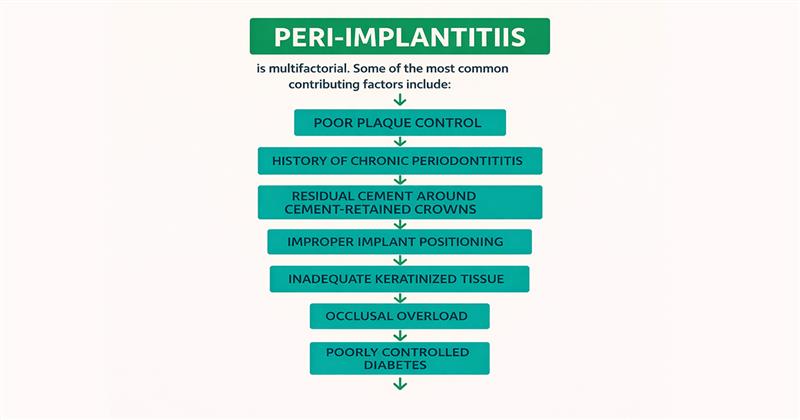
Why Peri-Implantitis Develops
Peri-implantitis is multifactorial. Some of the most common contributing factors include:-
- Poor plaque control
- History of chronic periodontitis
- Residual cement around cement-retained crowns
- Improper implant positioning
- Inadequate keratinized tissue
- Occlusal overload
- Smoking
- Poorly controlled diabetes
In most cases, peri-implantitis results from a combination of biological and mechanical factors, not a single cause.
Goals of Peri-Implantitis Treatment
Whether you choose a non-surgical or surgical approach, the objectives remain the same: –
- Eliminate bacterial biofilm
- Reduce inflammation
- Halt further bone loss
- Maintain implant stability
- Improve long-term prognosis
The severity of disease determines which treatment approach will be effective.
Non-Surgical Management of Peri-Implantitis

When Is Non-Surgical Treatment Appropriate?
Non-surgical management is best suited for:
- Early peri-implantitis
- Shallow probing depths (≤5 mm)
- Minimal radiographic bone loss
- Patients with good oral hygiene compliance.
It is often the first line of treatment, especially in early diagnosis.
Components of Non-Surgical Therapy
1. Mechanical Debridement
Mechanical removal of plaque and calculus from implant surfaces is the foundation of non-surgical care.
Commonly used instruments include: –
- Curettes such as Titanium, Plastic or Carbon.
- Ultrasonic scalers with implant-safe tips.
The goal is to disrupt the biofilm without damaging the implant surface.
2. Antimicrobial Therapy
Antimicrobials are used as an adjunct, not a replacement, for mechanical cleaning.
Options include:
- Chlorhexidine gels and mouth rinses.
- Local antibiotic delivery systems (minocycline, doxycycline).
- Systemic antibiotics in selected cases.
These help reduce bacterial load and inflammation.
3. Air-Polishing Systems
Air-polishing with low-abrasive powders such as glycine or erythritol has gained popularity because: –
- It is minimally invasive
- It effectively removes biofilm
- It preserves implant surface integrity
- It improves patient comfort
This method is particularly useful during maintenance therapy.
4. Occlusal Adjustment
Excessive occlusal forces can accelerate peri-implant bone loss.
Non-surgical management should include:
- Check for premature contacts.
- Adjusting occlusion if required.
- Managing bruxism or parafunctional habits.
Ignoring occlusion can compromise treatment outcomes.
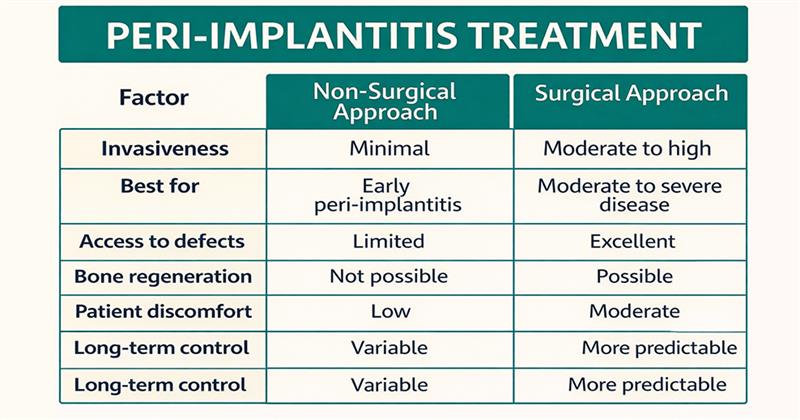
Advantages of Non-Surgical Treatment
- Minimally invasive
- Cost-effective
- Reduced patient discomfort
- Shorter chair time.
- Ideal for early disease.
Limitations
- Limited access to deep defects
- Ineffective in advanced bone loss
- Often insufficient for long-term stability in severe cases
Non-surgical therapy can control disease but may not always resolve it completely.
Surgical Management of Peri-Implantitis
When Is Surgical Intervention Required?
Surgery becomes necessary when:
- Probing depths exceed 5–6 mm
- Radiographic bone loss is significant
- Non-surgical therapy fails
- Implant surfaces are heavily contaminated
At this stage, conservative treatment alone is usually inadequate.
Types of Surgical Approaches
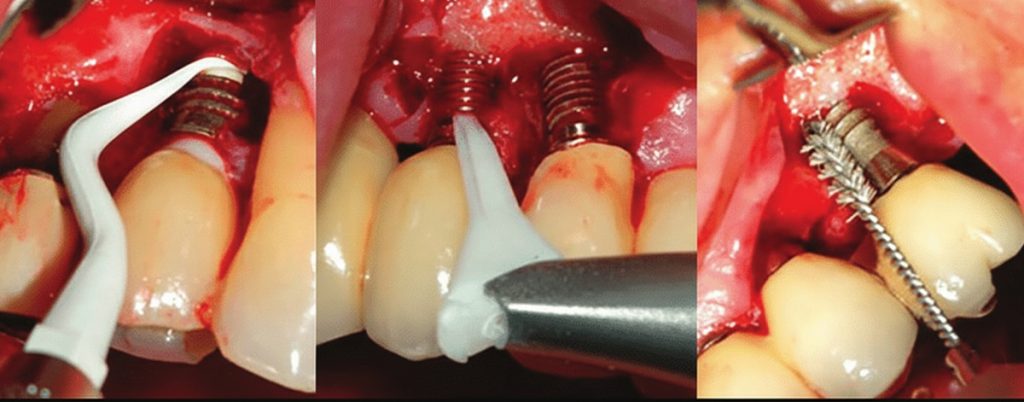
1. Open Flap Debridement
This involves:
- Elevation of a flap to expose the implant surface.
- Complete removal of granulation tissue.
- Thorough decontamination of implant surfaces.
It provides direct access to deep defects that cannot be cleaned non-surgically.
2. Implant Surface Decontamination
Various methods are used to clean exposed implant surfaces, including:
- Mechanical instruments
- Air-abrasive systems
- Laser therapy
- Chemical agents such as hydrogen peroxide or citric acid
The aim is to reduce bacterial contamination without damaging the implant.
3. Resective Surgery
Resective procedures include:
- Removal of inflamed tissue.
- Bone recontouring.
This approach is commonly used in non-esthetic areas where regeneration is not feasible.
4. Regenerative Surgical Approach
In selected cases, bone regeneration may be attempted using:
- Bone graft materials
- Barrier membranes
- Growth factors
Regenerative surgery is most successful in containing defects and esthetic zones.
Advantages of Surgical Treatment
- Better access to infected areas
- More predictable results in advanced cases
- Potential for bone regeneration
- Improved long-term implant survival
Limitations
- Higher cost
- Longer healing time
- Increased patient discomfort
- Technique-sensitive procedure
Surgical vs Non-Surgical Approach:
Importance of Maintenance Therapy
No treatment will succeed without long-term maintenance.
Key elements include: –
- Regular professional cleanings
- Reinforcement of oral hygiene instructions
- Periodic radiographic evaluation
- Monitoring probing depths
- Smoking cessation counseling
Maintenance visits are often scheduled every 3–6 months, depending on patient risk factors.
Clinical Insight for Dentists
The earlier peri-implantitis is diagnosed, the more conservative the treatment can be. Delaying treatments often lead to surgical complexity and reduced implant survival.
Final Thoughts
Peri-implantitis is a growing challenge in implant dentistry, but it is manageable with the right approach. Non-surgical therapy works well in early stages, while surgical intervention becomes essential in advanced cases.
Successful management depends on: –
- Early detection
- Proper case selection
- Patient compliance
- Structured maintenance protocols
Ultimately, peri-implant health is a shared responsibility between the clinician and the patient.
Frequently Asked Questions (FAQs)
Bone loss cannot be fully reversed, but disease progression can be controlled and stabilized.
No. Antibiotics are adjunctive and should not replace mechanical debridement.
Implants should be evaluated every 3–6 months based on an individual risk.
Surgical outcomes depend on defect type, implant surface, and patient compliance.
Yes, if left untreated, it can result in complete implant failure.



No Comment