How to Set Up an Efficient Sterilization Protocol for Small Clinics
Introduction
In a small dental practice, the stakes for infection control are just as high as in a major hospital. Sterilization is the foundation of patient safety, staff protection, and strict legal compliance. However, efficiency is often the secondary challenge; in a limited space with a small team, a clunky protocol can bottleneck your entire daily schedule.
An optimized sterilization workflow does more than just kill pathogens-it preserves your instrument investment, minimizes overhead costs, and ensures that clinical operations move forward without delay. Even with lower patient volumes, there is no margin for error when it comes to the “sterile chain.”
Understanding Sterilization vs. Disinfection
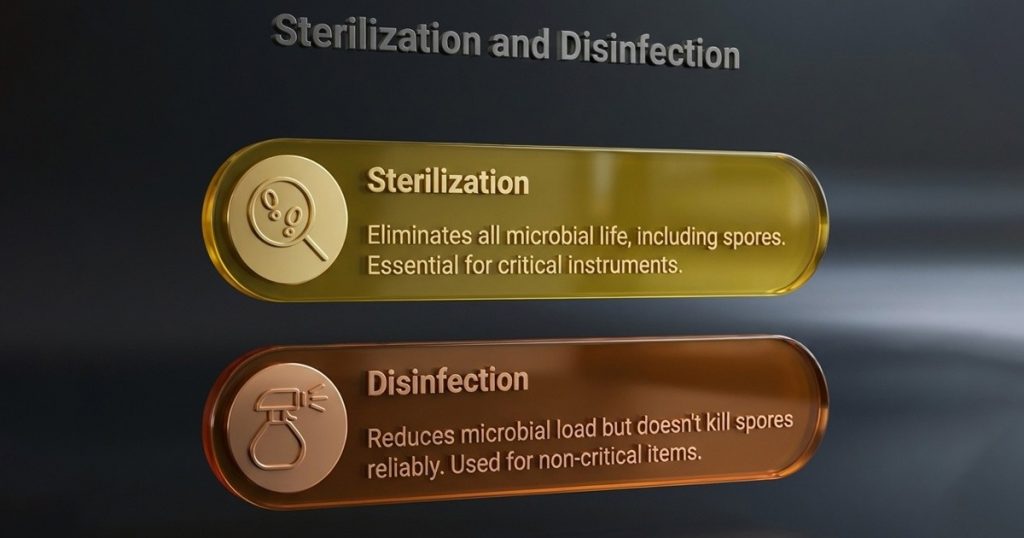
The Pro-Tip: High-level disinfectants are often viewed as a “shortcut,” but they are slower, more technique-sensitive, and less reliable than a validated sterilization cycle.
Key Principles for Small Clinics
Efficiency in a small space relies on discipline and design rather than expensive automation.

Choosing the Right Sterilization Methods
Small clinics must balance speed, instrument compatibility, and footprint.
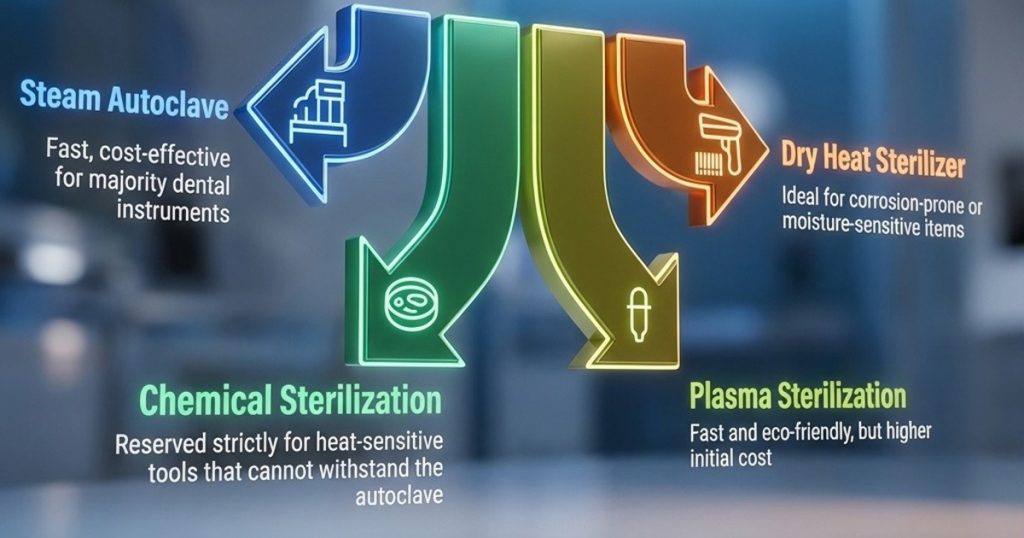
Pro-Tip: Combining a chemical pre-clean (enzymatic soak) with autoclaving improves the removal of bioburden and ensures the steam reaches every surface of the tool.


Product- Waldent Self-Seal Sterilization Pouches
Designing an Efficient Sterilization Workflow
A system-wide approach is always more effective than focusing on individual instruments.
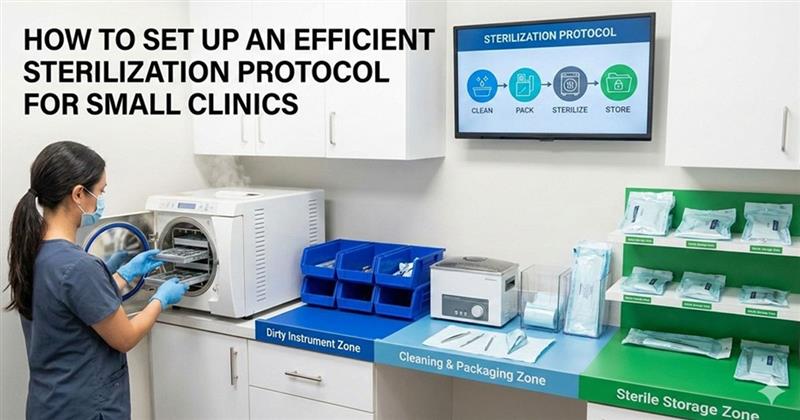
Workflow Planning & Zoning
- Physical Separation: Clearly mark zones. The “Dirty” zone is for de-bridement; the “Clean” zone is for packaging; the “Sterile” zone is for storage and cooling.
- Load Scheduling: Avoid “half-loads” unless necessary. Syncing cycles with your patient load prevents the “instrument bottleneck” during busy afternoon blocks.

Staff Training & Safety
- PPE Compliance: Staff must utilize heavy-duty utility gloves, masks, and eye protection during the cleaning phase to prevent percutaneous injuries.
- Competency Checks: Conduct quarterly reviews. A simple mistake in wrapping a cassette can render an entire cycle non-sterile.

Equipment & Surface Management
- Right-Sizing: Choose an autoclave chamber size that matches your daily instrument volume. An oversized unit wastes energy, while an undersized unit creates delays.
- High-Touch Surfaces: Focus disinfection on light handles, x-ray buttons, and chair controls using EPA-registered hospital disinfectants.
- Anti-Retraction Valves: Ensure handpieces are equipped with these valves to prevent the “suck-back” of oral fluids into the internal lines.



Products: Durr Dental ID 213 Disinfectant Solution For Instruments, Waldent Schuster Class B Autoclave 23L
Monitoring, Validation, and Traceability
- The Triple Indicator Rule:

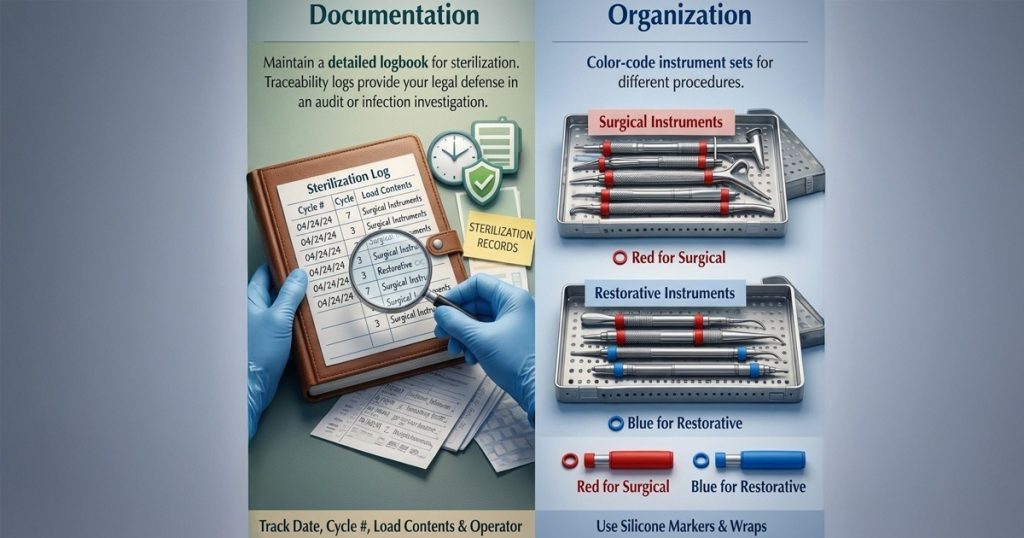
- Documentation: Maintain a detailed logbook. In the event of an audit or a post-operative infection, your traceability logs (Date, Cycle #, Load Contents, Operator) are your only legal defence.
- Organization: Use color-coded silicone markers or wraps to distinguish between different procedure types (e.g., Red for Surgical, Blue for Restorative).
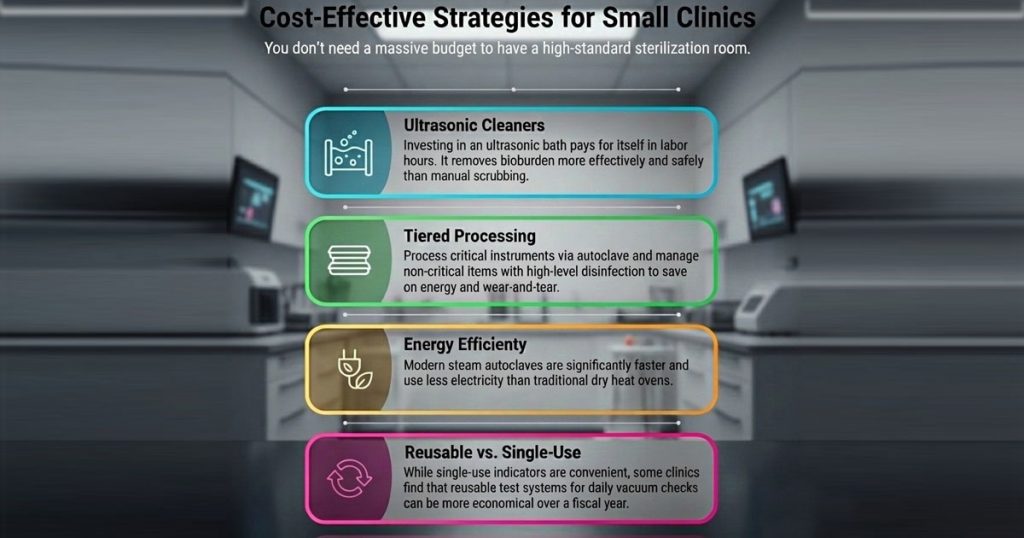
Cost-Effective Strategies for Small Clinics
Common Mistakes to Avoid

Conclusion
An efficient sterilization protocol is the silent engine of a successful dental practice. By structuring your workflow, training your team to respect the “unidirectional flow,” and maintaining meticulous logs, even the smallest clinic can achieve hospital-grade safety. Not only does this protect your patients and your license, but it also creates an organized environment where the clinical team can focus on what they do best: patient care.
FAQ’s
Sterilization is crucial to ensure patient safety, staff protection, and legal compliance. An efficient sterilization protocol also helps preserve your instruments and minimizes overhead costs.
Sterilization is the process of eliminating all forms of microbial life, while disinfection reduces harmful microorganisms but doesn’t guarantee complete elimination. Sterilization is a more reliable method for infection control.
The key is designing a disciplined workflow with clearly marked zones: Dirty, Clean, and Sterile. Planning the workflow and avoiding “half-loads” will help minimize delays and keep things organized.
The Triple Indicator Rule involves using three types of indicators (chemical, biological, and physical) to ensure that sterilization conditions are met. This helps verify that the sterilization cycle was effective.
Maintain detailed logs of each sterilization cycle, including the date, cycle number, load contents, and operator. This documentation is crucial in case of audits or post-operative infections.




No Comment