Management of Medical Emergencies in Dentistry

Medical emergencies in dental practice may be rare, but when they do occur, they demand immediate and effective action to prevent potentially serious consequences. It is essential for dental professionals to be well-versed in recognizing the early signs and symptoms of common emergencies and to respond promptly with appropriate management. In this blog, we will explore the most frequently encountered medical emergencies in dentistry, their clinical presentations, and practical steps for effective management to ensure the safety and well-being of patients.
Common Medical Emergencies and their Management in Dentistry:
1. Vasovagal Syncope
Syncope is one of the most commonly encountered medical emergencies in dental practice. It is defined as a sudden, transient loss of consciousness with spontaneous recovery. Extreme anxiety, fear, and pain are common factors that contribute to this condition.
Signs and Symptoms:
- Light-headedness
- Dizziness
- Pallor
- Nausea
- Sweating
- Visual disturbances
- Fainting
- Slow pulse due to bradycardia and hypotension
Management:
- Stress reduction
- Good communication and reassurance
- The patient should be positioned in a supine position with legs slightly raised.
- Aromatic ammonia should be used as a respiratory stimulant, as it helps increase cerebral perfusion, allowing the patient to regain consciousness.
- The airway should be assessed.
- Oxygen may be administered if necessary, using a Ventimask or nasal cannula.

2. Hyperventilation
At times, the patient might start breathing rapidly and deeply due to anxiety or fear. This conscious overdrive of ventilation is known as hyperventilation. It can lead to excessive washout of carbon dioxide, causing a decreased partial pressure of arterial carbon dioxide (PaCO2 below 35 mm Hg). Hypocapnia causes constriction of cerebral blood vessels, producing light-headedness and dizziness.
Signs and Symptoms:
- Palpitations
- Tachycardia
- Trembling and sweating
- Anxiety
- Tingling
- Muscular twitching and carpopedal tetany-like features due to hypokalemia and hypocalcemia
Management:
- Reassurance
- Breathe slowly and normally
- The only emergency in which oxygen therapy should NOT be given
- The old treatment of rebreathing into a paper bag should be strictly avoided
- Breathing through cupped hands in front of the nose is recommended
- Alternatively, breathing through a detached oxygen mask with holes for the release of excessive CO2 should be used
- In refractory cases, sedation with diazepam or midazolam may be required

3. Asthma/Bronchospasm
Asthma is characterized by an increased contractile response of smooth muscles in the small airways. In a dental setting, it may be triggered by anxiety, aerosolized particulate matter, or certain drugs, such as aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs).
Signs and Symptoms:
- Coughing and wheezing
- Dyspnea
- Hunger for air
Management:
- Known asthmatic patients should be instructed to carry their bronchodilator medications, in the form of an inhaler, at the time of their appointment
- In case of an asthmatic episode, the patient should be seated upright, and oxygen should be administered via mask or nasal cannula
- The patient should be asked to take puffs from their own inhaler or a salbutamol inhaler from the emergency kit
- Puffs from the inhaler should be repeated every 5 minutes or until symptoms improve
- In status asthmaticus, IV salbutamol (100 mg) and IV hydrocortisone should be administered to help prevent relapse
- 0.3 mg of IM epinephrine can be used as a last resort or when IV access is not available to relieve bronchospasm
- All asthma patients should be given oxygen at a rate of 4-6 L/min using a face mask
- Oxygen saturation should be monitored with a pulse oximeter and maintained above 90%
- Medical help should be sought in case of life-threatening signs, such as non-resolving wheezing, cyanosis, bradycardia, slow respiratory rate, and deteriorating mental status

4. Allergic Reaction/Anaphylaxis
An allergic reaction is an antigen and antibody reaction to a substance (allergen) to which the patient has been previously sensitized. There can be various types of allergic reactions, ranging from life-threatening type I allergic reactions (anaphylaxis) to type IV (delayed hypersensitivity).
Signs and Symptoms:
- Skin allergy, resulting in itching, redness, and skin rash
- Severe bronchospasm if the lungs are involved
- Laryngeal edema and laryngeal spasm in some cases
- Nausea
- Vomiting
- Diarrhea
- Rhinitis
- Conjunctivitis
- Urticaria
- Antigen-mediated vasodilation, leading to hypotension and potentially cardiac arrest
Management:
- Pheniramine maleate (Avil) is the drug of choice when the allergic reaction is slow in onset and predominantly involves the skin. It is given intramuscularly in a dose of 22.5–45 mg, followed by oral administration of 25 mg 3–4 times a day for 2 days.
- For bronchospasm and laryngeal edema, early use of epinephrine is recommended. The adult dose is 0.3 mg IM (1:1,000), or when venous access is available, 1–3 ml of diluted 1:10,000 is injected slowly over 5 minutes.
- The dose should be titrated carefully due to potential side effects of epinephrine, such as severe hypotension and fatal arrhythmias.
- Epinephrine is the only drug in the emergency kit that is kept preloaded due to its urgency.
- The patient should be made aware of the allergen so that future contact with it is strictly avoided.
5. Hypoglycemia and Hyperglycemia
Hypoglycemia and hyperglycemia are common medical emergencies faced by patients with diabetes mellitus. In a dental setting, hypoglycemia is more common than hyperglycemia.
Signs and Symptoms of Hypoglycemia:
- The skin of a hypoglycemic patient is cold and wet
- Loss of consciousness
- Blood pressure is high
Signs and Symptoms of Hyperglycemia:
- The skin of a hyperglycemic patient is flushed and dry
- Blood pressure is low
- These patients may have a fruity, sweet odor on their breath due to ketoacidosis
Management:
- The most common cause of hypoglycemia is a missed meal, so ensure the patient never misses a meal before dental treatment.
- If hypoglycemia is evident, give glucose or any sugary source for the patient to drink or chew if they are conscious.
- For an unconscious patient, 25–50 mL of 50% dextrose should be administered intramuscularly (IM).
- Vital signs should be monitored, and basic life support (BLS) should be provided if necessary.
- The emergency management of a hyperglycemic patient is supportive in nature within the dental clinic. For definitive management, the patient should be taken to a nearby hospital.
6. Angina/Myocardial Infarction
Chest pain due to inadequate blood supply to the heart may be caused by angina or myocardial infarction. This typically results from narrowing or spasm of a coronary artery.
In angina, chest pain is directly related to stress, anxiety, or physical exertion. The episode is usually brief and settles within 5 minutes, with no permanent damage to the heart. Acute myocardial infarction (MI) occurs due to the development of a clot in one of the coronary arteries, leading to a lack of blood supply to part of the heart muscle, causing permanent damage.
Common Signs and Symptoms of both conditions:
- Chest pain
- Shortness of breath
- Nausea
- Vomiting
- Pain radiating to the shoulders, arms, neck, jaw, or upper abdomen
Management:
- Administer supplemental oxygen via mask or nasal cannula.
- Nitroglycerin is the single most effective vasodilator used to relax the vascular smooth muscle in cases of angina pectoris. It can be given in the form of sublingual tablets or spray. A 0.4 mg tablet is placed sublingually every 5 minutes, with a maximum of three tablets over 15 minutes.
- Nitroglycerin is contraindicated if the patient has concurrent hypotension.
- In cases of acute myocardial infarction, it is recommended that, outside the hospital, patients receive antifibrinolytic aspirin in a dose of 150–325 mg.
- The patient should be transferred to the care of a cardiologist as early as possible.
7. Seizure
A seizure, or convulsion, is an episode of abnormal electrical activity in the brain, resulting in an attack involving changes in consciousness, motor activity, or altered sensory phenomena.
Signs and Symptoms:
- In a typical tonic-clonic seizure, major skeletal muscles contract, and the patient loses consciousness.
- The patient may become apneic, cyanotic, and may bite their tongue.
- Involuntary, powerful movements make the patient susceptible to injuries.
- The postictal phase is characterized by drowsiness, fatigue, and confusion.
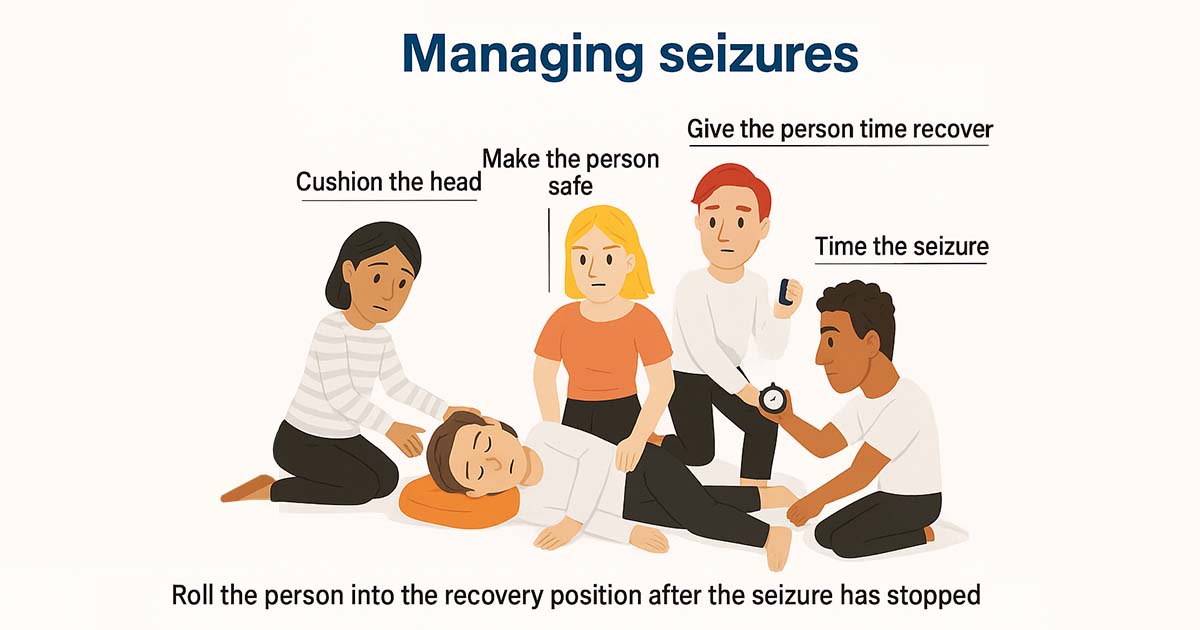
Management:
- Never attempt to restrain the patient’s movements or place any object in their mouth during a seizure.
- The patient should be gently turned onto their side to protect the airway, and protective padding may be placed under the head to prevent injury.
- After the seizure, continue to monitor the airway and vital signs.
- Oxygen can be administered via mask or nasal cannula, if required.
- In the case of status epilepticus, diazepam 10 mg should be administered intravenously, slowly over a 2-minute period to stop seizure activity.
- For children, diazepam is given in a dose of 0.2–0.5 mg/kg IV.
- The patient should be referred to their neurologist as soon as possible for further evaluation and treatment.
8. Drug Overdose Reaction
An excessive dose, inadvertent intravascular injection, or rapid administration of a drug may cause undesirable drug effects. Overdose of local anesthetic agents is one of the commonly seen medical emergencies in dental clinics.
Read Also: Dental Local Anesthesia: Essential Insights for Every Dentist
Signs and Symptoms of Lidocaine Toxicity/Overdose:
- Restlessness
- Agitation
- Confusion
- Blurred vision
- Ringing or buzzing in the ears (tinnitus)
- Muscle fasciculations, tremors, or seizure activity
Management:
- In cases of lidocaine toxicity, airway and circulation should be maintained.
- Administer oxygen and monitor vital signs continuously.
- Basic life support (BLS) measures should be instituted.
- There is no specific antidote for lidocaine toxicity; supportive measures should be continued until the drug is metabolized.
- For benzodiazepine overdose, Flumazenil is the specific antagonist that reverses the sedative effects of midazolam and diazepam.
- Flumazenil is available as 0.1 mg/mL in 5–10 mL multidose vials.
- The dosage for reversal is 0.2 mg (2 mL) administered IV every 1–2 minutes, up to a maximum of 1 mg.
- The patient should be observed for about an hour after reversal due to the risk of re-sedation or recurrence of symptoms.
9. Choking/Foreign Body Aspiration
Choking is one of the medical emergencies seen in dentistry in which there is accidental slippage of a dental instrument, extracted tooth, or dental material into the oropharynx thus leading to choking or foreign body aspiration. About 90% of swallowed objects pass through the gastrointestinal tract without complications. However, in the case of sharp objects (e.g., a reamer or file), a gastroenterologist should be consulted immediately.
Signs and Symptoms:
- Mild obstruction leads to a coughing reflex, and the object may be expelled by coughing.
- Severe obstruction results in a weak or ineffective cough; the patient may not be able to breathe, speak, or cry.
Management:
- If the object is visible in the oropharynx, it can be retrieved using Magill’s forceps or a high-volume suction apparatus with a suction tip.
- The patient should be encouraged to cough and expectorate the object if possible.
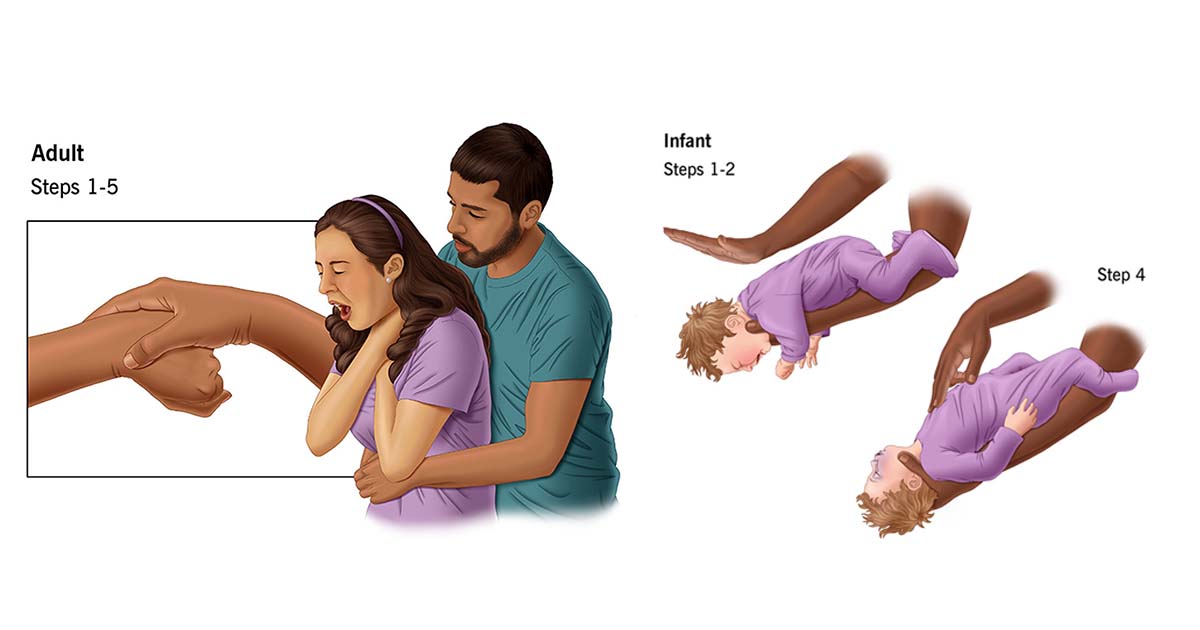
- One of the recommended maneuvers for severe airway obstruction is the Heimlich maneuver (abdominal thrusts) to help expel the foreign body.
- Children under 1 year of age may require a combination of back slaps and chest thrusts, while maintaining a head-down position.
- If these procedures are unsuccessful, surgical intervention should be considered to secure the airway.
10. Hypotension
Low blood pressure (systolic pressure below 90 mm Hg) can lead to inadequate cerebral perfusion and loss of consciousness. The most common cause of a hypotensive episode in a dental setting is vasovagal syncope, which is typically associated with bradycardia (pulse below 50 beats per minute).
Management:
- Changing the patient’s position to supine with the legs elevated usually results in recovery.
- When hypotension is accompanied by bradycardia, such as in vasovagal syncope, atropine is a useful drug. It is administered in a dose of 0.5 mg IM or IV, and can be repeated every 6 minutes, up to a maximum of 3 mg, depending on heart rate and blood pressure readings.
- Ephedrine is another drug helpful in increasing systolic pressure in patients with a normal heart rate. It can be administered as 25 mg IM or sublingually.
- Phenylephrine may be used to manage hypotension in patients who have a normal or elevated heart rate (tachycardia).
11. Hypertension
Hypertension may be encountered in patients experiencing extreme pain, anxiety, or restlessness during lengthy dental procedures.
Management:
- The patient should be asked to remain calm and reassured.
- If the episode is accompanied by symptoms such as chest pain, headache, or visual disturbances, drug intervention to reduce blood pressure may be required.
- Known hypertensive patients who have missed their medication should be given their usual dose of antihypertensive drug, if appropriate.
- Esmolol, a selective beta-1 blocker, can be used to manage an acute hypertensive episode.
Conclusion:
Medical emergencies in dentistry, though uncommon, can arise without warning and require swift, knowledgeable responses to ensure patient safety. By understanding the signs, symptoms, and appropriate management of these conditions, dental professionals can minimize risks and improve outcomes. Staying prepared with the right training and equipment is essential for effective emergency care.
Dentlkart supports dental practitioners by providing reliable emergency drugs and dental supplies, helping you maintain a safe and well-equipped practice at all times.

1 Comment
Thank you for knowledge
Good 👍