Internal Hex vs Conical Implant Connections: A Clinical Guide

In modern implantology, we often focus on thread design or surface macro-topography. However, the long-term success of a restoration frequently hinges on what happens at the “handshake”-the implant–abutment interface. This connection directly influences mechanical stability, peri-implant bone behaviour, and prosthetic longevity.
While Internal Hex and Conical Connections dominate the market, their clinical behaviour differs significantly. Understanding where and why each performs better is essential for achieving predictable outcomes in daily practice.
Understanding Implant–Abutment Connections
At its core, the connection defines how forces are transferred from the prosthesis to the bone. An ideal connection should prioritize:
- Mechanical stability to withstand masticatory cycles.
- A minimal microgap to prevent bacterial colonization.
- Reduced micromovement to protect the internal components.
- Preservation of crestal bone for long-term esthetics and health.
The Clinical Reality: Most implant failures related to prosthetics originate at the implant-abutment interface, not within the implant body itself. If the connection fails, the osseointegration is eventually put at risk.
Internal Hex Connection: Design & Concept
The Internal Hex features a hexagonal recess inside the implant body. It was designed to provide anti-rotational stability, which is especially useful during the critical phase of abutment placement.
Key Characteristics:
- Defined Indexing: Allows for easy orientation and prosthetic handling.
- Screw-Retained Stability: The system relies on the tension of the abutment screw to keep components together.
- Universal Use: One of the most widely used and compatible systems globally.
Clinical Insight: Internal hex connections distribute occlusal forces primarily to the screw. This increases the clinician’s reliance on screw preload; if that tension is lost, the system is prone to instability.

Product: Impact DSI Internal Hex Dental Implant 6mm
Conical (Morse Taper) Connection: Design & Concept
A Conical Connection uses a tapered, friction-fit mechanism (typically between 6 to 12 degrees) to unite the implant and abutment. Unlike a standard flat-to-flat interface, the primary stability here comes from the wedging effect of the cone.
Key Design Feature:
- Active Taper Zone: The upper portion of the connection features the conical seal.
- Sub-Crestal Hex: A hexagonal index is present, but it is located downwards, below the active taper area. This allows for precise prosthetic positioning (indexing) without interfering with the conical seal’s function.
These connections are frequently paired with platform switching to move the microgap away from the bone crest.
Key Characteristics:
- Cold-Weld Effect: The friction-fit creates a mechanical interlock that virtually eliminates micromovement.
- Superior Seal: Because the connection relies on the conical taper rather than the hex for the seal, it provides an excellent barrier against bacterial infiltration.
- Wall-Centric Loading: Forces are distributed to the sturdy implant walls rather than just the screw, reducing the risk of screw loosening.
Less Known Fact: True Morse taper connections can achieve bacterial seal levels comparable to natural tooth cementum junctions. By placing the hex below the tapered zone, the design ensures that the seal remains hermetic even if the hex itself is not perfectly tight, significantly reducing the risk of peri-implantitis.

Products: Apex Konnect Dental Implants 5.0mm, Apex Konnect Dental Implants 3.50mm
Key Differences: Hex vs. Conical Implant
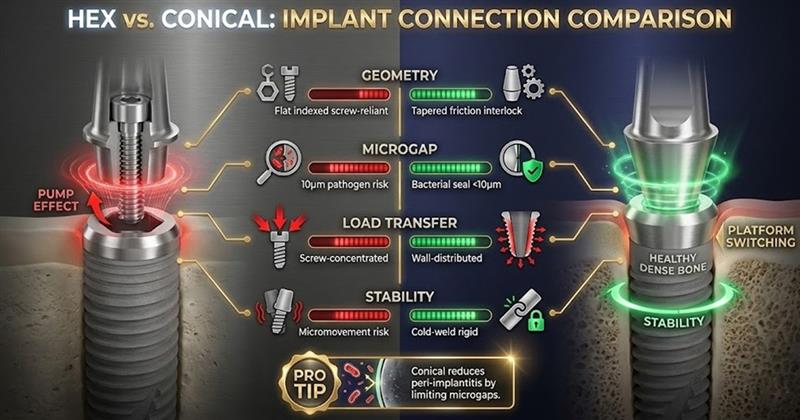
1. Geometry & Engagement
- Internal Hex: Uses geometric, indexed engagement. It is easy to “feel” when the abutment is seated, but it relies almost entirely on the screw to resist lateral loads.
- Conical: Uses tapered friction-fit with a hexagonal index located below the active taper area. It relies on mechanical interlocking, which reduces the mechanical burden on the screw.
2. Microgap & Bacterial Seal
- Internal Hex: The microgap may increase under functional load (the “pump effect”).
- Conical: The taper design limits microgap formation and bacterial infiltration.
- Pro Tip: Microgaps as small as 10 µm can harbor peri-implant pathogens; conical designs are engineered to stay below this threshold.
3. Load Transfer & Stress Distribution
- Internal Hex: Forces are transmitted mainly through the abutment screw.
- Conical: Forces are distributed along the internal walls of the implant body. This improved stress distribution is a key factor in crestal bone stability.
4. Stability & Micromovement
Micromovement is the leading cause of screw loosening. While the Internal Hex has a higher potential for micromovement in high-load posterior cases, the Conical Connection’s “cold-weld” effect keeps the interface rigid.
Advantages of Each Type
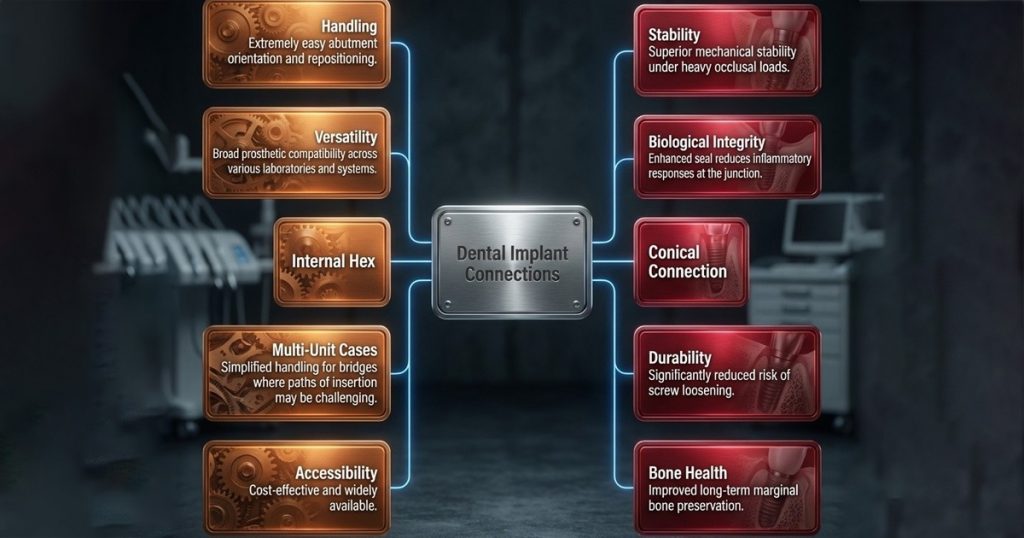
Maintenance & Reliability
Maintenance burdens should influence your system selection. Internal Hex systems generally require more frequent periodic screw monitoring, whereas Conical Connections often see a lower frequency of prosthetic maintenance visits.
Best Clinical Applications: When to Use Which Implant?
Choosing the right connection is a site-specific decision. Below is a quick decision guide for your next case:
| Clinical Scenario | Preferred Connection | Why? |
|---|---|---|
| Single Posterior Tooth | Conical | Manages heavy occlusal loads; resists screw loosening. |
| Esthetic Zone (Anterior) | Conical | Protects crestal bone; essential for papilla support. |
| Multi-Unit Bridge | Internal Hex | Easier indexing and path of insertion for multiple units. |
| Full-Arch (Fixed) | Internal Hex | Standardized components simplify complex prosthetic steps. |
| Bruxers / Parafunction | Conical | Minimizes micromovement under extreme stress. |
| Beginner Clinicians | Internal Hex | High tactile feedback during seating; less technique sensitive. |
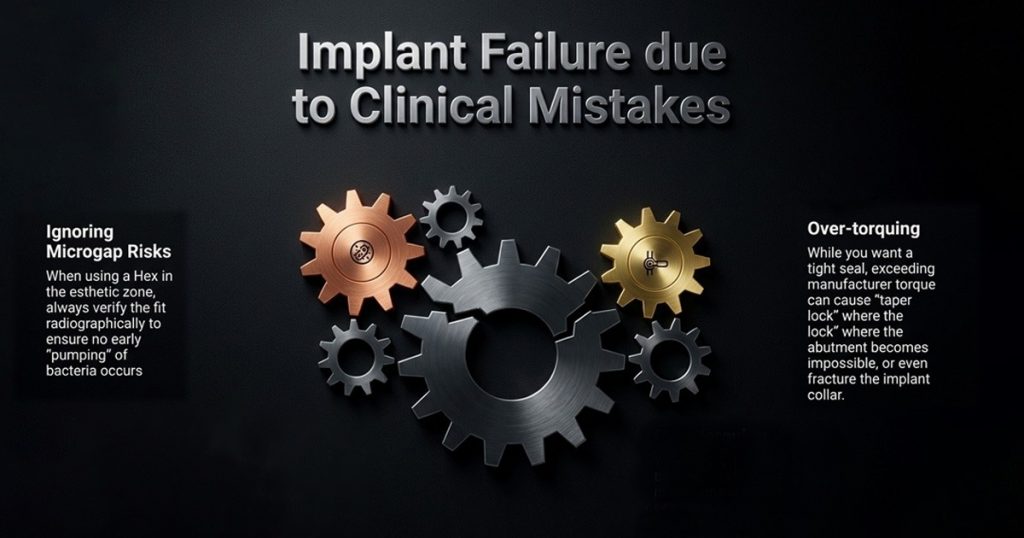
Clinical Mistakes to Avoid
Conclusion
Ultimately, the choice between Internal Hex and Conical Connection systems is not a matter of universal superiority, but of specific clinical application. While Internal Hex implants offer proven versatility and familiarity, Conical Connections excel in delivering superior mechanical integrity and biological stability where long-term precision is paramount. For the advanced implantologist, this selection should never be based on trends, but rather guided by a rigorous evaluation of case selection, occlusal demands, and the patient’s biological risk profile. In modern implantology, connection design remains a critical biomechanical decision, not merely a branding choice.
FAQ’s
The implant–abutment connection plays a critical role in mechanical stability, load transfer, and bacterial sealing. Most prosthetic complications begin at this interface, and failure here can eventually compromise osseointegration and crestal bone health.
The Internal Hex connection is designed to provide anti-rotational stability and easy indexing during abutment placement. Its predictable geometry makes prosthetic handling straightforward, especially in complex or multi-unit restorations.
In Internal Hex systems, occlusal forces are primarily transferred to the abutment screw. This means the stability of the entire restoration relies heavily on maintaining adequate screw tension, making the system more prone to screw loosening if preload is lost.
Conical connections use a tapered friction-fit that creates a “cold-weld” effect between the implant and abutment. This mechanical interlock minimizes micromovement by distributing forces along the implant walls rather than concentrating them on the screw.
The tapered design of Conical connections significantly reduces microgap formation, even under functional load. By positioning the hex below the active taper zone, the seal remains intact, limiting bacterial infiltration and lowering the risk of peri-implantitis.


No Comment