Infection Control Practices for Dentists

As dentists, we are deeply committed to ensuring optimal infection control for our patients, often going to great lengths to maintain a safe environment. However, in our dedication to patient safety, we sometimes overlook the critical need to prioritize our health and well-being. While infection control measures for patients and dentists often overlap, there are instances where our health may be at risk due to lapses in maintaining personal infection control practices.
In this blog, we delve into essential strategies to enhance infection control measures tailored for dentists, empowering you to safeguard your health without compromising patient care.
Why are infection control practices important for dentists?
Infection control practices are essential for dentists’ health. Due to daily exposure to saliva, blood, and other secretions during procedures, dentists face a tenfold higher risk of infection than other healthcare professionals. Implementing effective infection control measures is crucial to prevent the spread of diseases to patients and staff, significantly reducing occupational hazards.
Prioritizing infection control not only protects dentists’ health but also creates a safer work environment, allowing them to focus on providing quality care without the constant worry of infections. When patients recognize that their dentist takes infection control seriously, it builds trust and encourages them to return for their oral care.
Moreover, adhering to these practices is vital for maintaining medical licensure and avoiding legal repercussions. A strong reputation for high infection control standards can set a practice apart, attracting new patients and fostering loyalty among existing ones. Ultimately, prioritizing infection control is key to safeguarding dentists’ health and ensuring the success of their practices.
Personal Protective Measures
Personal protective measures encompass two essential components: personal protective equipment (PPE) and immunization. PPE includes wearable equipment specifically designed to shield dental professionals from exposure to infectious agents during patient care.
It effectively protects personal clothing and skin likely to be soiled with blood, saliva, or other potentially infectious materials. Key components of PPE include head covers, gloves, surgical masks, gowns, and more.
Here’s a detailed overview of the key protective measures:
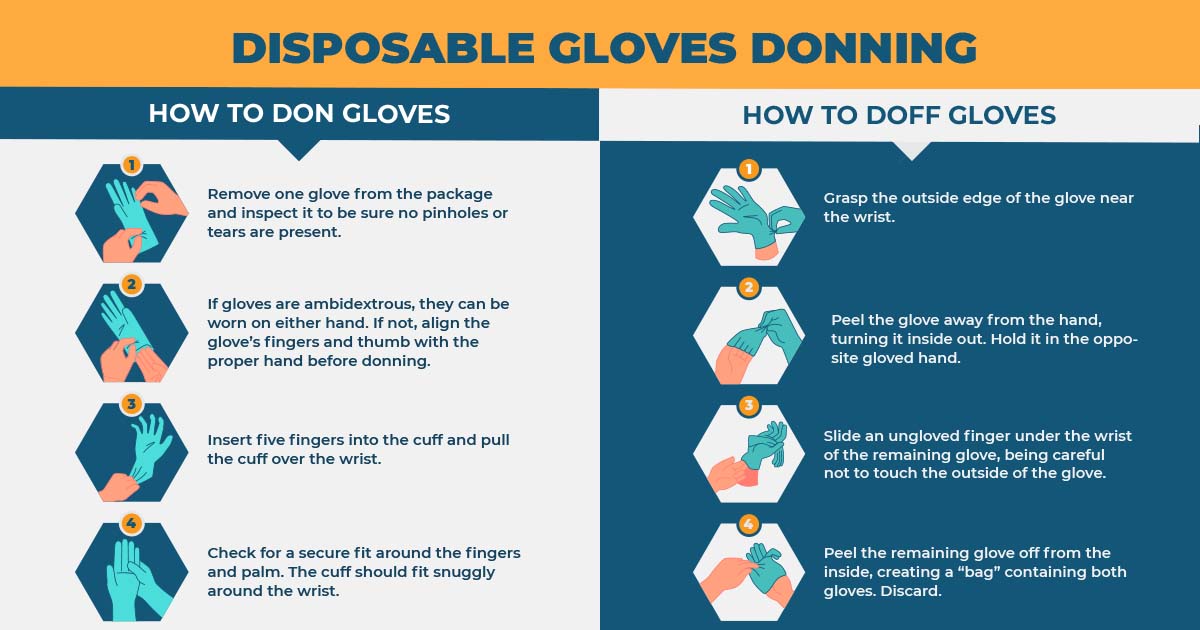
1. Gloves:
The most important worn PPE is quality vinyl gloves. Changing gloves after every use and performing hand hygiene methods like handwashing before touching any item, environmental surfaces, eyes, nose, or mouth, or starting with another patient is extremely important. Gloves should properly fit but not restrict any movement and should cover the cuffs of a long-sleeved gown. Care should be taken to avoid injury during procedures. If gloves get torn, cut, or punctured they must be changed immediately before continuing with the procedure.
Healthcare workers with a past of reported allergies to latex or the powder used in gloves which may be as irritation contact dermatitis, delayed contact dermatitis(rash), and immediate allergic urticaria. Cotton glove liners can be used to provide a barrier between the skin and the latex in such cases. Alternatively, non-latex gloves (vinyl, nitrile or other nonsynthetic polymer) can also be used.
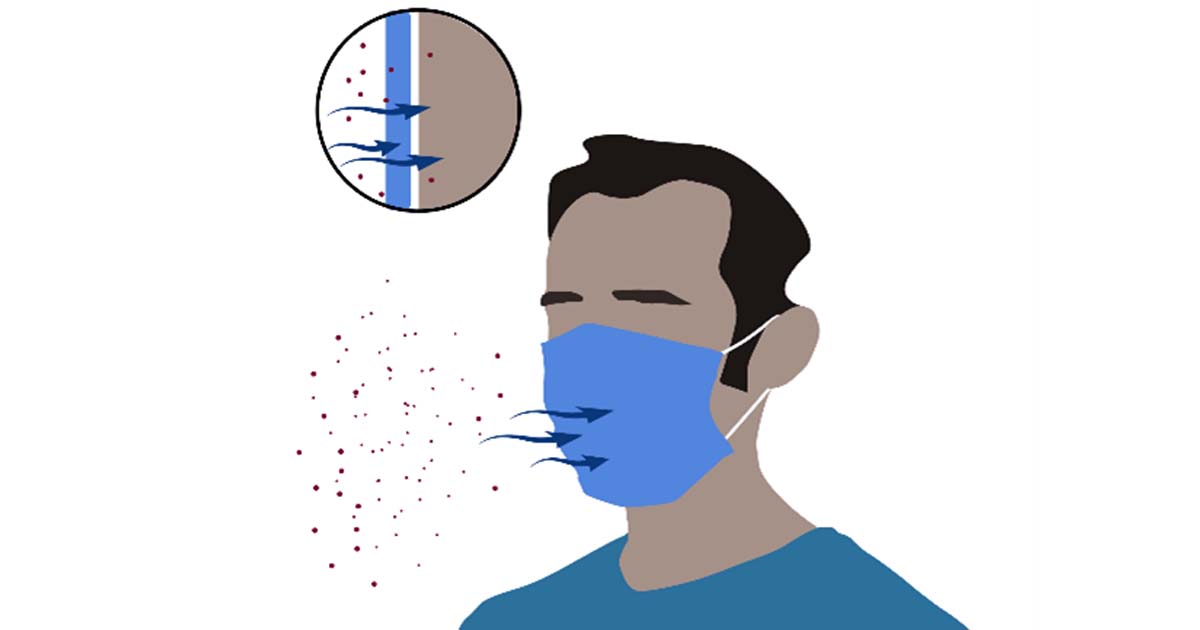
2. Surgical Masks:
These protect the nose and mouth from likely splashes and sprays of blood or body fluids. Splashes and sprays can be generated from a client’s behavior (e.g. coughing or sneezing) or during procedures (e.g. suctioning, irrigation, cleaning equipment).
Masks with a fluid-resistant membrane layer help prevent fluid absorption into the layers of the mask. Surgical masks with ear loops are the easiest to put on and prevent transmission of microorganisms to dentists. Dental aerosols that are generated can be smaller than 5 microns in diameter and thus the masks should prevent the passing of these aerosols from the outer layer to the inner layer.
Dentists should thus use 3-ply or 4-ply surgical masks to prevent any amounts of microorganisms from reaching their mouth or body as a whole for the best protection.
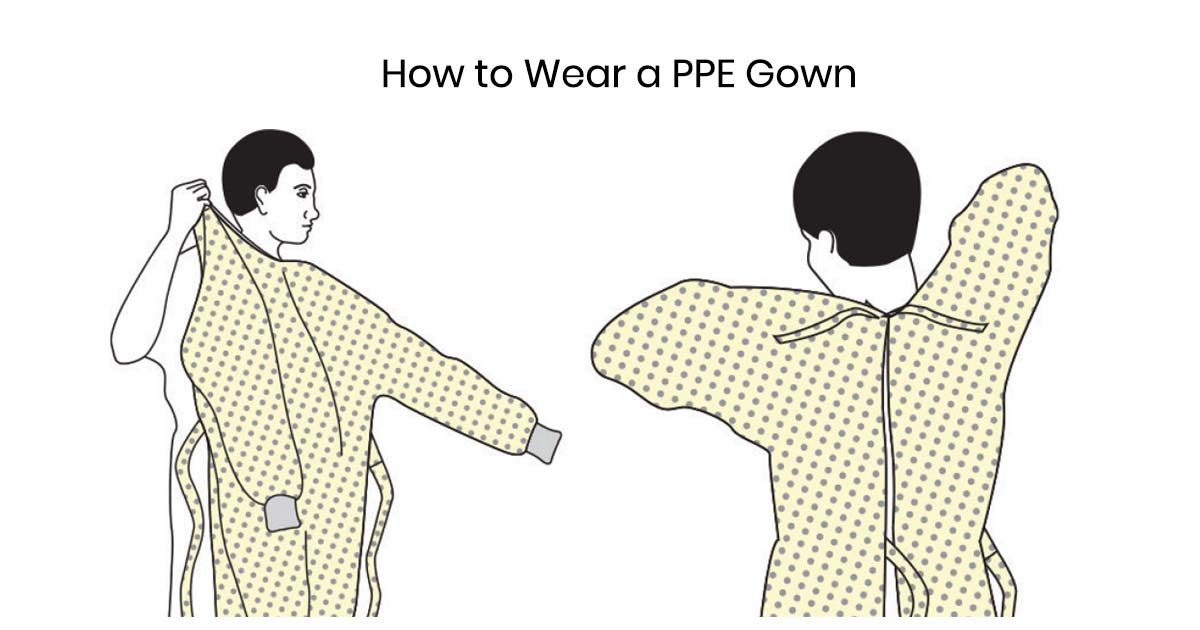
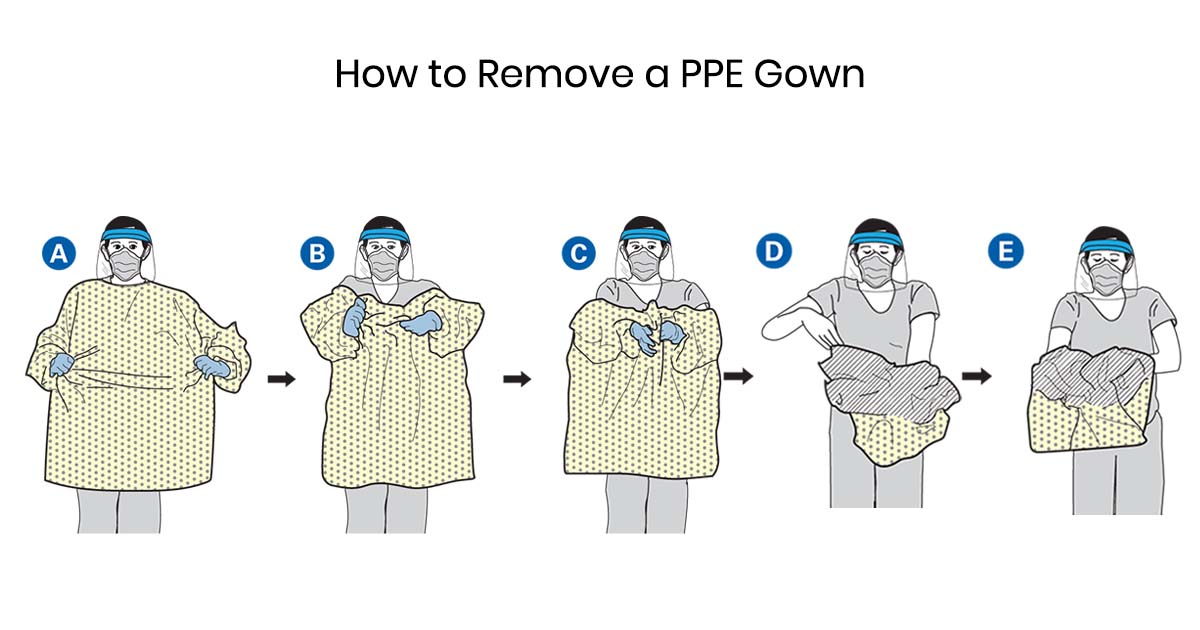
3. PPE Gowns:
To put on a gown should be the first procedure followed by mask and eye protection. These gowns should be long-sleeved and leave no skin uncovered to protect from likely splashes, and sprays during procedures and client care activities. These should be changed after every patient to control cross-contamination between patients. Surgical gowns should be routinely worn by dentists and assistants alike while working chairside in a dental office or a laboratory.
Read Also: Sterilization in Dentistry: Safeguarding Oral Health
4. Protective eyewear and shield:
Eye injuries might occur from projectiles such as bits of calculus during scaling procedures and splatters from body fluids while using high-speed handpieces and another potential source of eye injury is the intense dental curing light.
Dentists can use polycarbonate glasses with side shields, face- shields, and glasses with disposable side shields to protect them from the above-mentioned incidences during clinical hours. These can also help them to protect their eyes during the trimming of casts and dentures, cutting wires, and processing of instruments while working in a dental lab.

5. Immunization:
Dentists are often at risk of getting in contact with vaccine-preventable infections. Immunization against Hepatitis B, Varicella, Measles, Mumps, Rubella, Pertussis, and Viral influenza must be done at the required time intervals.
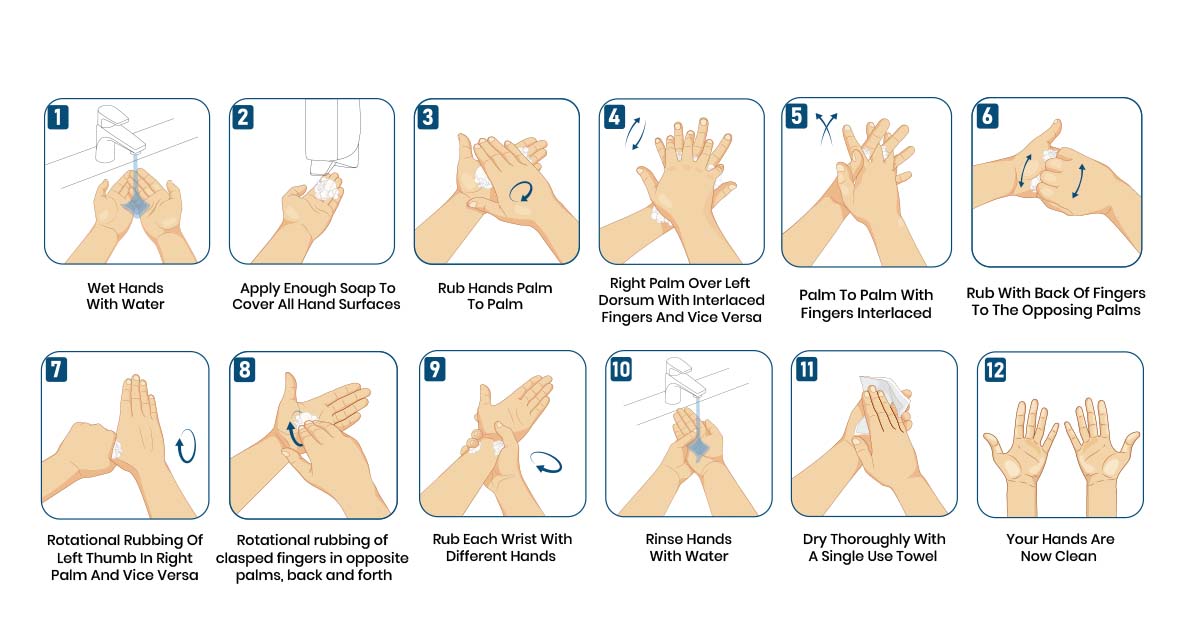
Hand Hygiene
Appropriate hand hygiene can minimize microorganisms acquired on the hands during daily duties and when there is contact with blood, body fluids, secretions, excretions, and known and unknown contaminated equipment or surfaces. Hands can become contaminated with infectious agents through contact with a patient, the patient’s surroundings, the environment, or other healthcare workers. Effective hand hygiene must be maintained and can be done in the following way:
1. Regular hand washing with normal soap and water
2. Anti-septic hand washing with antiseptic soap and water
3. Alcohol-based hand rub containing ethanol or isopropanol alcohol in a concentration between 60- 95%.
4. Surgical antisepsis is usually performed before a surgical procedure.
How to prevent air-borne disease transmission from a patient?
Patients with a chance of spreading airborne diseases require added precautions when visiting a clinic for their treatment. Other than the standard precautions following can be kept in mind:
- Ask the patient to only come to the clinic if it is an absolute necessity. Avoid scheduling an appointment till the patient is rid of all the symptoms.
- If need be, the patient should be given an appointment as the last patient to reduce the spread of infection to other patients and to also give you ample time to be ready with necessary precautionary measures.
- Hydrogen peroxide according to the new literature states that it reduces the infection load in the saliva. Hence, a mouth rinse containing the same can help in reducing the transmission of infection.
- Isolation with a dental dam should be performed to reduce the spread of aerosols.
- The surrounding environment should be cleaned twice.
What to do in case of needle puncture or bodily fluid Cross-contamination?

If a healthcare professional or an assistant gets punctured by a sharp object or by a needle that is contaminated with blood or any other bodily fluid, it is important that the necessary steps are taken to prevent any infection from the other person.
Following are some important measures that can be taken to prevent these:
- Once injured, immediate washing of the exposed site or wound should be done with soap and water.
- Alcohol-based hand rubs or solutions should be used if soap and water are not available.
- If working in an organization, inform the supervisor or the concerned authority about the accident and fill in the report about the accident so that a thorough investigation can be done regarding the same.
- Seek medical care in a hospital.
- Give the doctor a detailed history of the incident including when and how it happened, how deep the injury is, first aid methods used, etc.
- Blood tests for HBV, HCV, and HIV should be done as soon as possible. You should also be offered counseling about these tests before samples are taken.
- Inform the patient about the accident and consent should be taken for their blood tests for HIV, HBV, and HCV status. Counseling should be done for them too.
- Till the test results are released the healthcare professional should avoid blood donation and should practice safe sex.
- Post-exposure prophylaxis (PEP) may be recommended depending on the results and whether the source can be tested or not. These medications should be judiciously followed to prevent any infection. Furthermore, infectious disease specialists should be referred for further treatment.
Conclusion
Infection control practices are vital not only for patient safety but also for the health and well-being of dentists and their staff. As dental professionals, it is crucial to recognize that effective infection control measures protect against the significant risks associated with exposure to saliva, blood, and other bodily fluids encountered during routine procedures. By prioritizing personal protective equipment (PPE), such as gloves, masks, gowns, and eyewear, dentists can minimize their exposure to infectious agents and create a safer clinical environment.
Moreover, maintaining rigorous hand hygiene and staying up to date with immunizations are essential components of infection control that further safeguard both the dentist and their patients. Implementing these practices not only prevents the spread of infections but also fosters patient trust and enhances the overall reputation of the practice.
In the event of an exposure incident, it is imperative to follow established protocols promptly to mitigate risks and ensure appropriate medical care. By cultivating a culture of safety and vigilance in infection control, dentists can protect their health, maintain compliance with regulations, and ultimately ensure the success of their practices. In this way, effective infection control becomes a shared responsibility that benefits everyone in the dental care community.
Frequently Asked Questions:
Dentists are at a higher risk of infection due to frequent exposure to saliva, blood, and other secretions during procedures. Effective infection control measures protect both the dentist and patients from the spread of diseases, ensuring a safer work environment and fostering trust with patients.
Dentists should ensure immunization against the following:
· Hepatitis B
· Varicella (Chickenpox)
· Measles, Mumps, and Rubella
· Pertussis (Whooping Cough)
· Viral Influenza
· Wash the wound immediately.
· Inform your supervisor and seek medical care.
· Get tested for HBV, HCV, and HIV, and follow post-exposure prophylaxis if needed.
Dentists should wear:
· Gloves: Change after each use; use non-latex if allergic.
· Masks: 3-ply or 4-ply fluid-resistant to block aerosols and splashes.
· Gowns: Long-sleeved, changed after each patient.
· Eyewear: Polycarbonate glasses or face shields to protect eyes from splatters and projectiles.



No Comment