Bone Graft Materials Explained: Allograft vs Xenograft vs Synthetic

In the contemporary implant practice, the question is rarely if we should graft, but rather which matrix will yield the highest quality of vital bone for the specific defect at hand. As experienced clinicians, we know that successful osseointegration and long-term ridge stability are not merely products of surgical skill, but of biological synergy.
Material selection is a nuanced decision-making process that balances healing dynamics, defect morphology, and patient-specific physiological factors. This guide explores the mechanical and biological profiles of modern grafting materials to help refine your clinical protocols.
Material Profiles & Biological Behaviour
Understanding the “bio-logic” behind each material is the first step toward predictable hard tissue augmentation.
Allografts: The Biological Bridge
Derived from human donor bone, allografts (available as Mineralized Freeze-Dried Bone Allograft (FDBA) or Demineralized DFDBA) remain a staple in practice.

Properties: Primarily osteoconductive, but Demineralized Freeze-Dried Bone Allograft (DFDBA) offers osteoinductive potential by exposing Bone Morphogenetic Proteins (BMPs) during the demineralization process.
Clinical Nuance: While Bone Morphogenetic Proteins (BMPs) in DFDBA can accelerate the recruitment of osteoblasts, clinicians must account for the inherent variability between donor batches. Healing is typically faster than with xenografts, making it ideal for cases requiring shorter loading protocols.
Xenografts: The Structural Scaffold
Animal-derived matrices (typically bovine or porcine) are processed to remove all organic components, leaving a pure hydroxyapatite skeleton.
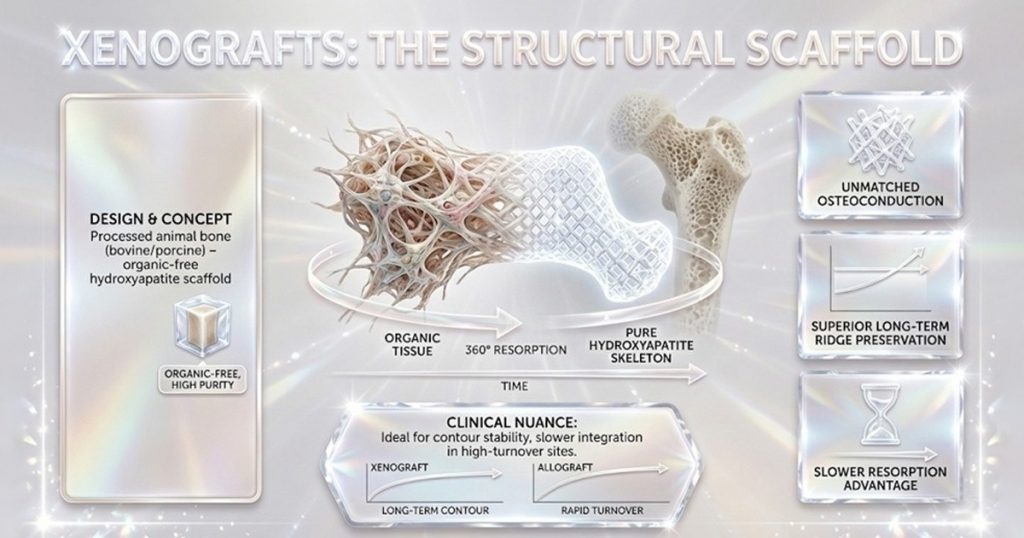
Properties: Excellent osteoconduction and unmatched long-term volume maintenance.
The Slower Resorption Advantage: Because xenografts resorb significantly slower than human bone, they are the gold standard for maintaining ridge contours over time. However, this same trait may delay full integration in high-turnover sites where rapid vital bone formation is the primary goal.
Products: MedPark S1 Bone Graft | Xenograft | Powder Type | 0.25gm | 0.2mm-1.0mm, Geistlich Bio-Gide
Synthetic Grafts: The Customizable Alternative
Synthetics, such as Hydroxyapatite (HA), β-Tricalcium Phosphate (β-TCP), or bioactive glass, offer an unlimited, infection-free supply.
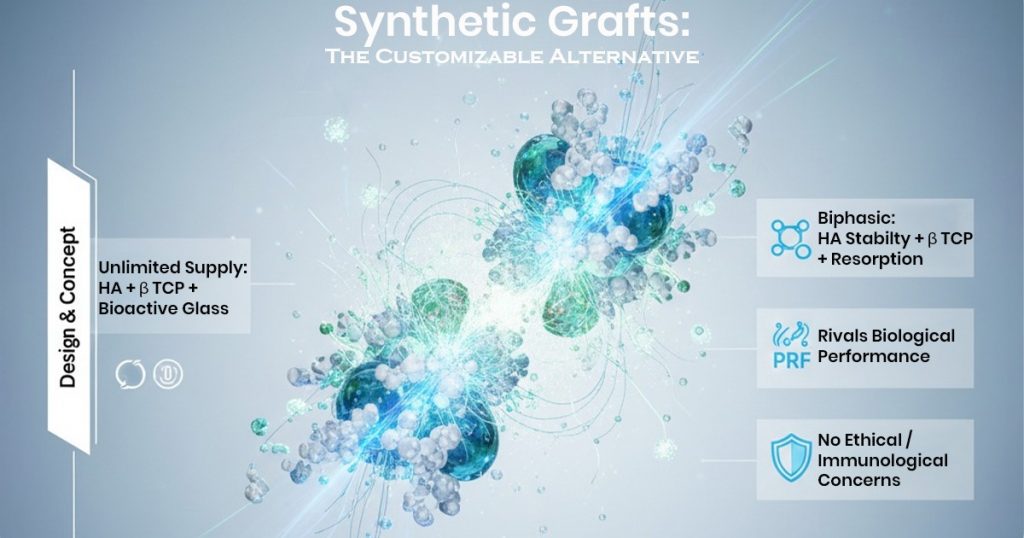
Clinical Tip: Modern synthetics are often biphasic, combining the stability of HA with the faster resorption of β-TCP. When combined with collagen or growth factors (like PRF), they can rival the performance of biological grafts without the ethical or immunological concerns.
Products: B-Ostin HA Nano Bonegraft Materials 0.355 – 0.500mm, Xcem Osspore Synthetic Bone Grafts HA / B-TCP Mix In Syringe
Key Factors Affecting Material Choice
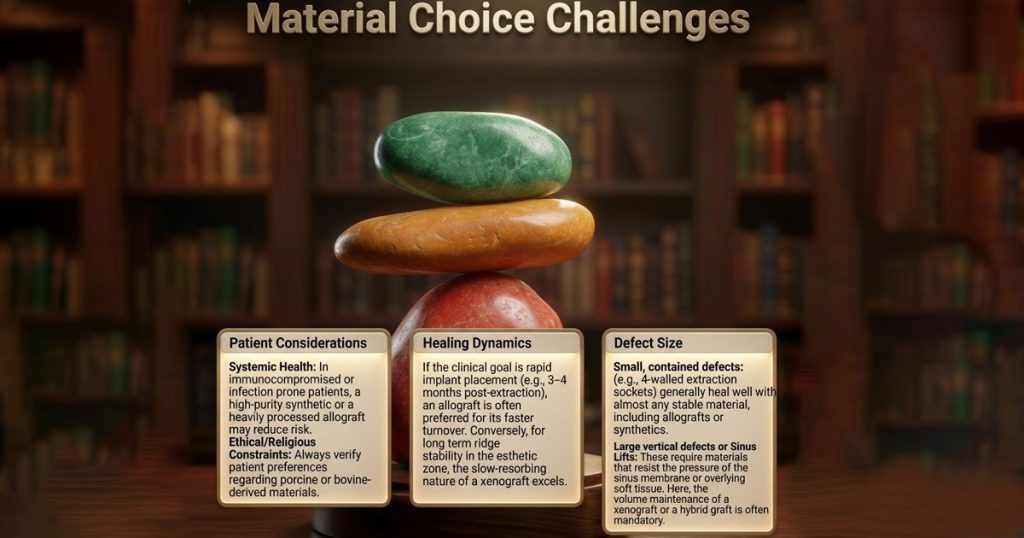
Practical Selection Guidelines
The following table serves as a quick-reference matrix for selecting graft materials based on clinical priorities.
| Material Type | Primary Mechanism | Resorption Rate | Best Used For… |
| Allograft | Osteoconductive / Osteoinductive | Moderate (3–6 months) | Faster turnover, predictable healing in moderate defects. |
| Xenograft | Osteoconductive | Very Slow (Years) | Sinus lifts, ridge volume maintenance, esthetic zone stability. |
| Synthetic | Osteoconductive | Variable (Engineered) | Patients with religious/ethical concerns; used in combination with biologics. |
| Hybrid | Dual Action | Balanced | Challenging GBR cases; provides both “speed” and “scaffold.” |
Conclusion
In modern implantology, no single graft material is universally superior. The “art” of bone grafting lies in matching the resorption rate of the material to the natural bone formation rate of the patient.
While Allografts offer biological speed and Synthetics offer safety and consistency, Xenografts remain unparalleled for volume stability. Increasingly, the Hybrid Approach-combining materials to leverage the benefits of each-represents the pinnacle of predictable surgical outcomes.
FAQs
No single graft material is universally ideal. Each case requires balancing biological behavior, mechanical stability, and healing timelines. In many advanced cases, combining materials offers the most predictable outcomes.
Material selection depends on defect size, morphology, and the desired healing timeline. Faster turnover cases favor allografts, while volume-critical sites like sinus lifts benefit from slow-resorbing xenografts. Synthetic or hybrid options are useful when patient or clinical constraints exist.
Allografts are preferred when quicker bone remodeling and earlier implant placement are required, such as in contained extraction sockets or moderate defects. Their faster resorption supports predictable vital bone formation within shorter loading protocols.
Modern biphasic synthetics can closely mimic natural bone healing, especially when combined with biologics like PRF or collagen. They offer consistency, safety, and are suitable for patients with ethical, religious, or immunological concerns.




No Comment