Scalpel vs. Laser Frenectomy: A Comprehensive Educational Guide
Frenectomy- the surgical removal or repositioning of restrictive oral frenum-are performed across all ages to improve speech, oral hygiene and orthodontic stability. For decades the standard method has been a simple scalpel excision with sutures. Over the last two decades, however, various surgical lasers have been introduced for soft tissue procedures. Clinicians therefore face a practical question: when is a laser the better tool, and when is a scalpel the reliable choice?
Understanding How Each Method Works
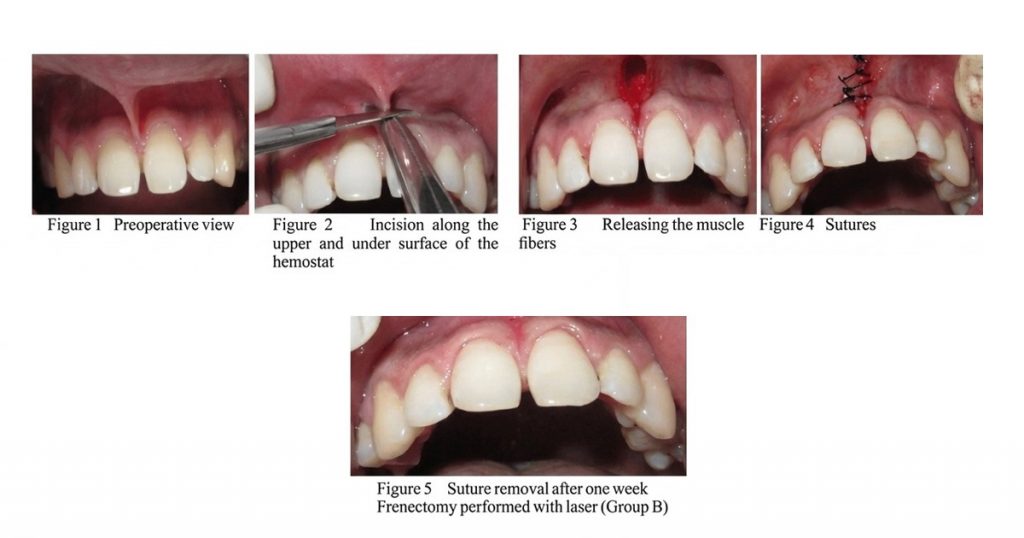
Conventional Scalpel Frenectomy
- Mechanical incision and excision: A scalpel cuts through the fibrous frenum, and the soft tissue is excised. The wound edges are then approximated with sutures, which control bleeding and stabilise the tissues.
- Haemostasis and suturing: Blood vessels are incised, so the surgeon must use pressure, vasoconstrictors or cautery, followed by suturing to achieve haemostasis. These steps extend operative time and contribute to postoperative swelling.
- Healing and scarring: Healing occurs by primary intention. The sutures and tissue manipulation can result in more noticeable scarring, especially when the frenum is thick or fibrotic.
- Equipment: Requires only sterile scalpels, sutures and basic surgical instruments. This makes the technique economical and widely accessible.
Products- Waldent Scalpel Blade Handle No. 3 (9/117), LifeShield Sterile BP Surgical Blades (Pack of 100)
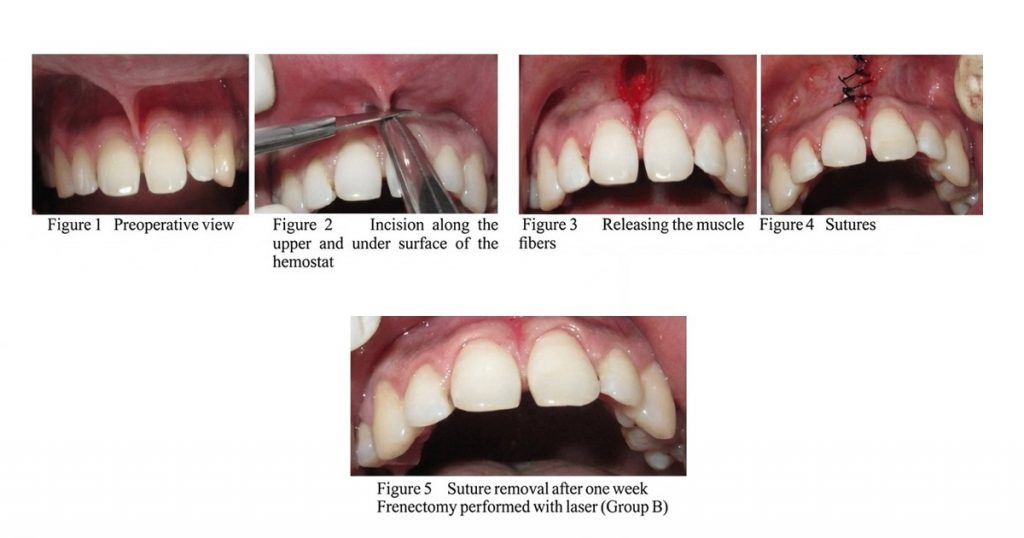
LaserAssisted Frenectomy
- Photothermal ablation: Lasers vaporise soft tissue through a concentrated beam of light. Different wavelengths-such as diode lasers (445 nm, 810 nm, 980 nm), CO₂ lasers (10.6 µm) and Er:YAG lasers (2.94 µm)-interact with tissue components like haemoglobin and water to varying degrees. This photothermal effect simultaneously seals blood and lymphatic vessels, reducing bleeding.
- Nerve sealing: The heat produced also seals sensory nerve endings, which lessens postoperative pain and reduces the need for analgesics.
- Minimal suturing: Because the laser coagulates wound margins, many cases heal by secondary intention without sutures. However, sutures may still be indicated for thick frena or when muscle fibres insert deeply.
- Safety and equipment: Lasers require appropriate training, eye protection and smoke evacuation. Proper power settings and technique are essential to avoid thermal injury to adjacent tissues.
Products: Woodpecker LX16 Dental Diode Laser, Soga iLaser 2 Dental Diode Laser
Clinical Outcomes and Procedural Considerations
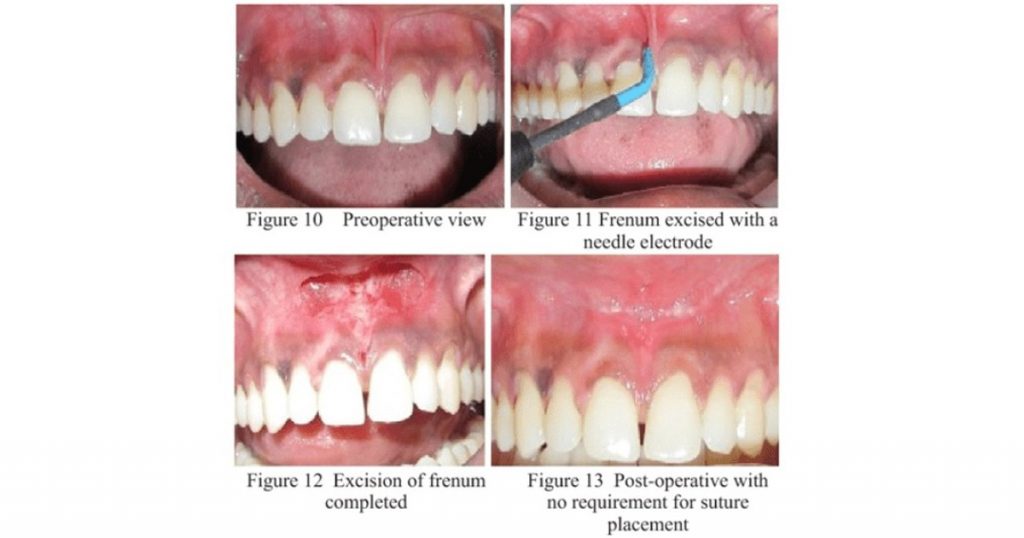
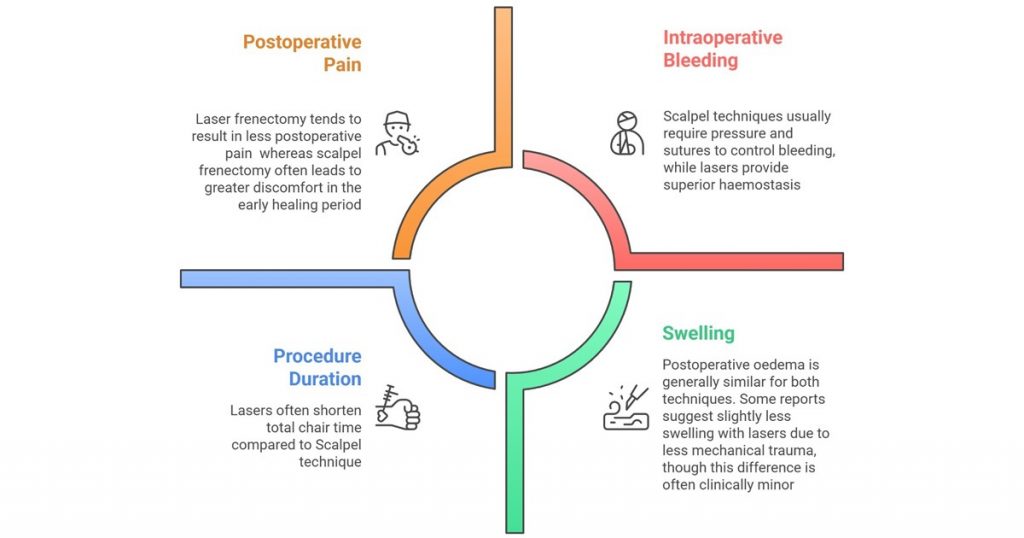
Pain, Bleeding and Surgical Time: What the Evidence Shows
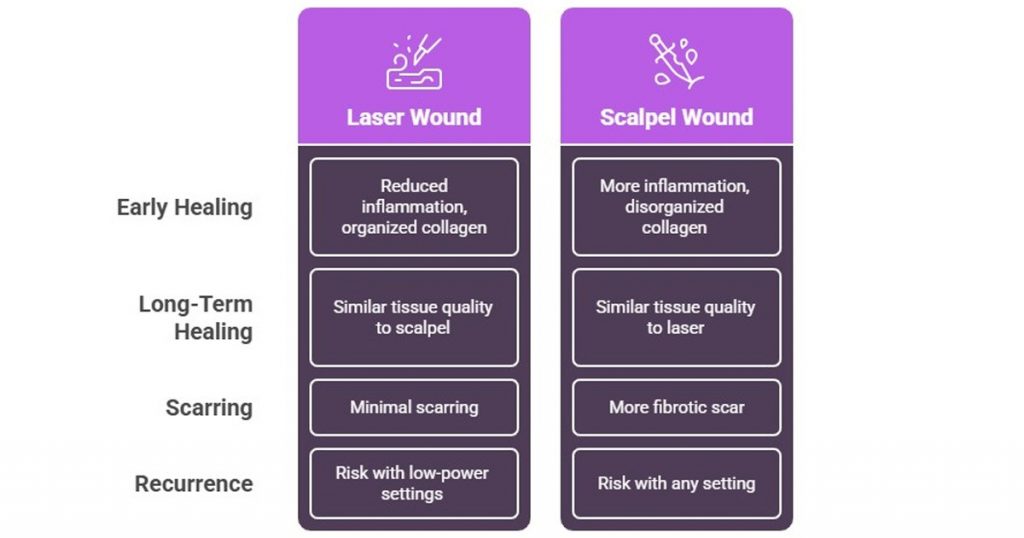
Healing Quality, Scarring and Histology
Patient Experience
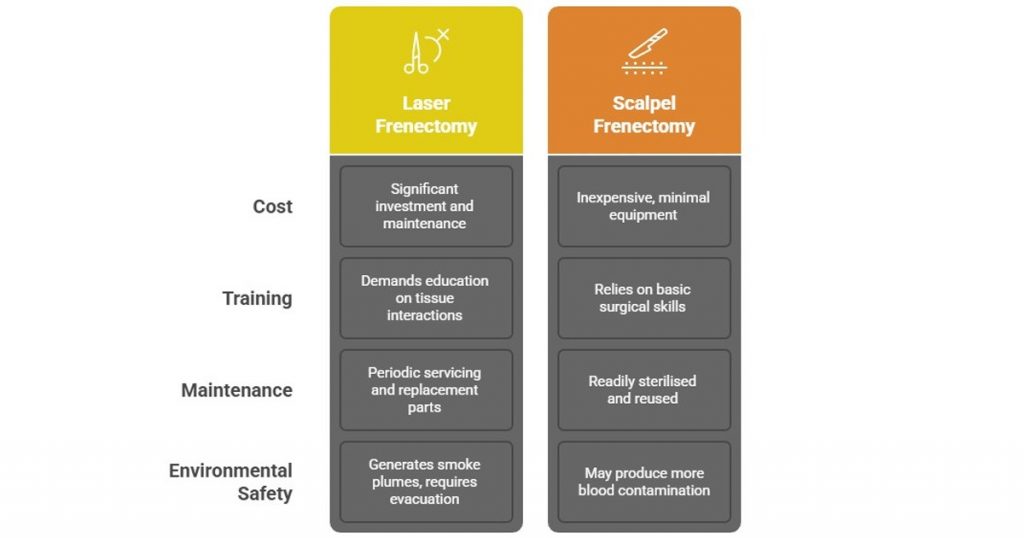
Cost, Training and Environmental Considerations
Indications and Case Selection
Choosing between scalpel and laser depends on:
- Anatomy: Thick or fibrotic frena with deep muscular insertions may respond better to a scalpel or a highpowered laser to ensure complete release.
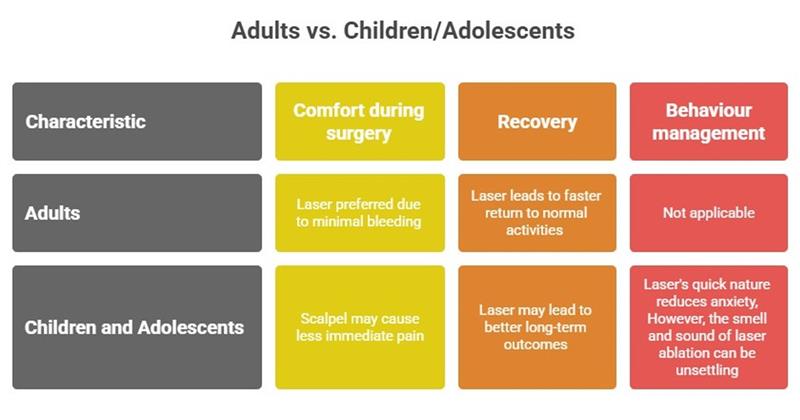
- Age: Laser procedures are attractive for children and adolescents due to reduced bleeding and short operating time. Adults often appreciate the comfort and aesthetics of lasers, while some paediatric patients may initially find the laser sounds and odour unsettling.
- Medical history: Patients with bleeding disorders or on anticoagulants benefit from the haemostatic nature of lasers. Pacemaker patients may require specific precautions.
- Resources: Scalpel surgery remains appropriate when budget or equipment availability limits laser use. Laser investment should reflect practice volume and patient demographics.
- Clinician expertise: Successful outcomes depend on surgical skill and familiarity with the chosen technique. Poor technique with either method can cause complications.
Safety and Potential Complications
- Thermal injury: Excessive laser power can char tissue and delay healing. Adequate training and conservative power settings reduce this risk.
- Smoke and fumes: Use effective evacuation systems and personal protective equipment to manage laser plume.
- Inadequate release: Incomplete removal of muscle fibres can lead to recurrence; thorough anatomical release is crucial.
- Operator error: Mishandling a laser can cause burns or damage to adjacent structures. Proper training is essential.
Decision Matrix
| Consideration | Scalpel | Laser | Notes |
|---|---|---|---|
| Bleeding control | Requires sutures and pressure; more bleeding | Excellent coagulation and visibility | Lasers useful for patients with bleeding risks |
| Postoperative pain | Moderate to high pain initially | Less pain during the first week | Differences diminish over time |
| Procedure duration | Longer due to suturing | Shorter; often eliminates need for sutures | Improved efficiency |
| Healing and scarring | Slower early healing; more scarring | Faster early healing; minimal scarring | Longterm outcomes similar |
| Cost and equipment | Low cost; widely available | High initial cost; requires training | Budget considerations |
| Learning curve | Basic surgical skills | Requires laser proficiency and safety measures | Training essential |
| Patient preference | Familiar technique | Often preferred for aesthetics and comfort | Personalised discussion advised |
| Recurrence risk | Low if muscle fully released | Higher if muscular release is incomplete | Thorough technique important |
Conclusion
Laser frenectomy provides compelling advantages in terms of reduced postoperative discomfort, excellent intraoperative haemostasis and faster early healing. Patients often favour the aesthetics and convenience of a bloodless, suturefree procedure, especially in paediatric cases where comfort and cooperation are crucial. Nevertheless, scalpel frenectomy remains a reliable, lowcost option that yields comparable longterm outcomes. The optimal technique depends on patient anatomy, systemic health, practitioner expertise and available resources. By understanding the strengths and limitations of each method, clinicians can tailor their approach to achieve the best functional and aesthetic results for every patient.
FAQ's
Yes, laser therapy tends to seal nerve endings during the procedure, resulting in less pain during the first postoperative week compared to scalpel techniques
Complete release of the muscle fibres is critical. Regardless of technique, inadequate release increases the risk of reattachment and functional relapse.
Laser is often preferred for children and adolescents due to faster procedures and minimal bleeding. However, younger patients may be sensitive to laser sounds or odours
Laser creates a dry, coagulated surgical site that may reduce microbial contamination. In contrast, scalpel wounds with bleeding and sutures might have a slightly higher risk of local infection.
Dr. Yashasvi Sharma
Author
Related Articles

Self-Etch vs. Selective-Etch vs Total-Etch: A Clinical Decision Guide for Everyday Restorations
IntroductionIn restorative dentistry, bonding success does not depend only on the composite resin or adhesive brand. More often than not, long-term success or f

Tissue-Level vs Bone-Level Implants: Clinical Selection Guide
In modern implantology, the debate isn't about which system is "better," but rather which design is most compatible with the patient’s specific anatomy. Implan

Paediatric Pulp Therapy: Guidelines & Best Materials (Pulpotomy / Pulpectomy)
Introduction to Pediatric Pulp Therapy In children, caries reaches the pulp fast because primary teeth have thinner enamel, dentin and larger pulp chambers.