
Guided Bone Regeneration (GBR): Steps, Indications & Products
Guided Bone Regeneration (GBR) is a surgical procedure focussed at restoring lost bone in areas of the jaw that have been damaged by injury, disease, or trauma. GBR is primarily used to create a stable foundation for dental implants. It involves the placement of a bone graft combined with a barrier membrane to direct the growth of new bone and prevent unwanted soft tissue from interfering with the regeneration process.
What is Guided Bone Regeneration (GBR)?

GBR is a surgical procedure that implant dentists use to regenerate lost bone. The procedure involves the placement of a barrier membrane over a bone graft to protect the healing area from soft tissue growth while allowing bone cells to grow in the right direction. Dentists often use GBR to restore bone in areas where there is insufficient bone volume for placing dental implants.
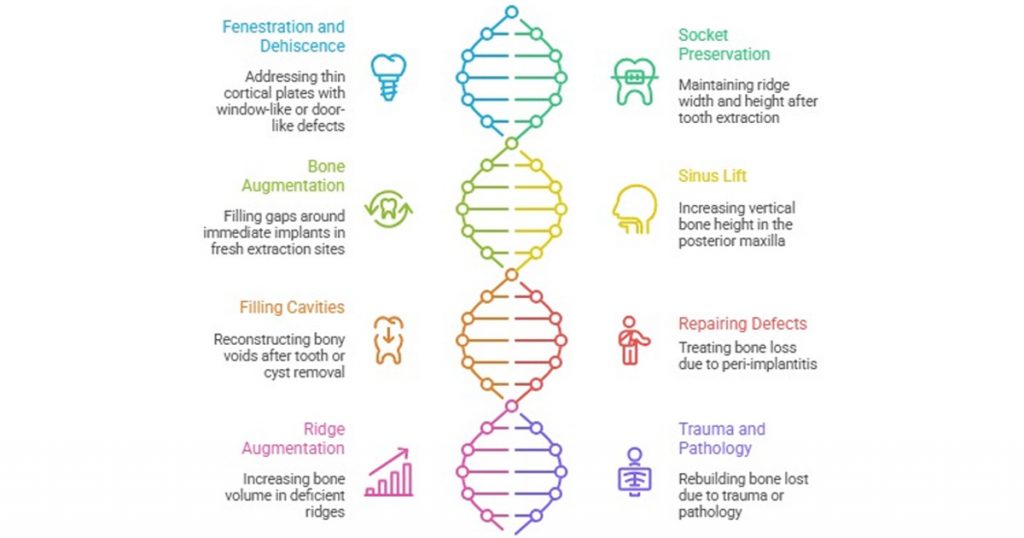
Indications for GBR
Clinicians indicate GBR in many situations where bone regeneration is necessary for successful implant placement. Some common indications include:
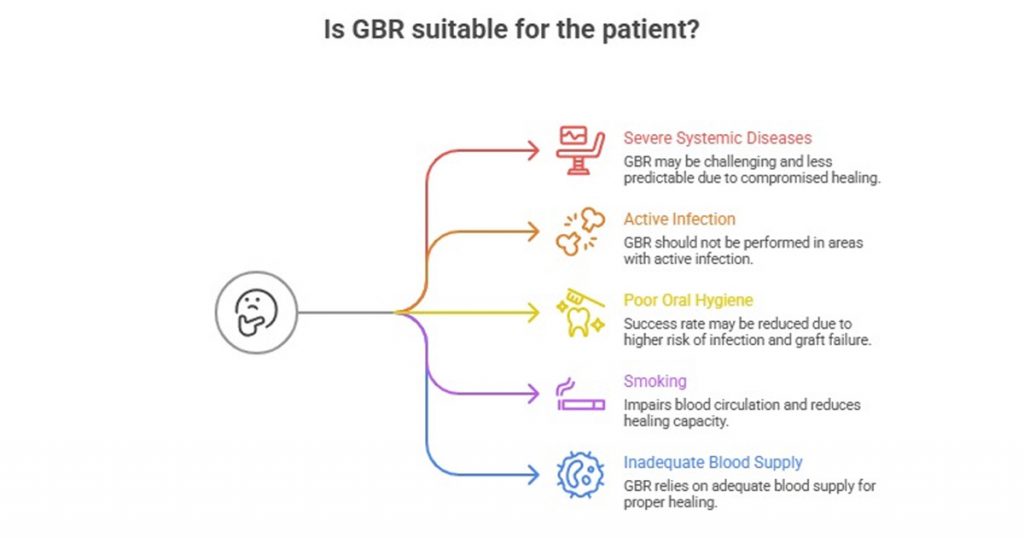
Contraindications for GBR
While GBR is an effective procedure, there are certain contraindications where it may not be suitable. These include:
Step-by-Step Process of Guided Bone Regeneration
Step 1: Pre-Operative Evaluation
Before performing GBR, the dentist will conduct a thorough evaluation that may include:
- X-rays or CT scans to assess bone loss.
- Clinical assessment of the site and patient health.
- Reviewing medical history to assess suitability for surgery.
Step 2: Anesthesia and Preparation
The clinician will numb the patient with local anesthesia and may use sedation in some cases to improve comfort. The team will sterilize the treatment area to minimize the risk of infection.
Step 3: Bone Graft Placement
The dentist will place the bone grafting material into the defect. This could be autogenous bone (taken from the patient), allograft (donor bone), or synthetic grafts. The graft material provides the foundation for new bone growth.
Step 4: Barrier Membrane Placement
The clinician places a barrier membrane over the graft to prevent soft tissue from interfering with bone regeneration. There are two main types of membranes:
- Resorbable membranes dissolve over time.
- Non-resorbable membranes require removal after healing.
Step 5: Suturing and Healing
After placing the membrane, the clinician carefully sutures the gums and advises the patient to avoid putting pressure on the area during healing. Healing time typically takes 3–6 months.
Step 6: Follow-Up Care
Clinicians require regular follow-up visits to monitor the healing process. The dentist may take additional X-rays to evaluate the bone regeneration and determine if the site is ready for implant placement.
Step 7: Implant Placement (Optional)
Once the bone regenerates, clinicians can place implants in the newly formed bone. This procedure may require additional healing time for the implant to properly integrate into the bone.
Recommended Products for GBR
1. Barrier Membranes
- Collagen Membranes: Biocompatible and resorbable, collagen membranes promote healing and integration.
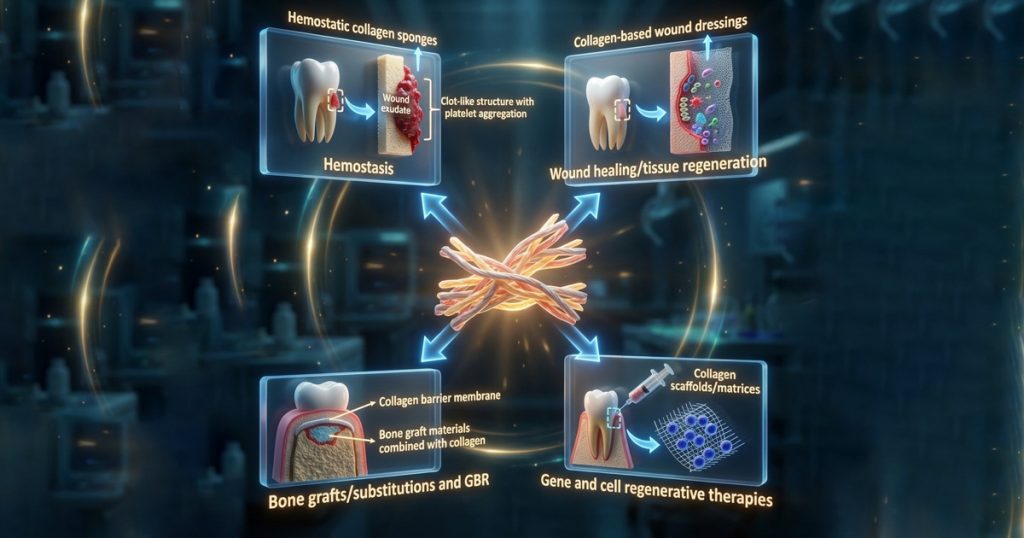
Recommended Product: Xcem Osspore Collagen Membranes
- ePTFE Membranes: Non-resorbable, these membranes provide excellent protection for the graft material.
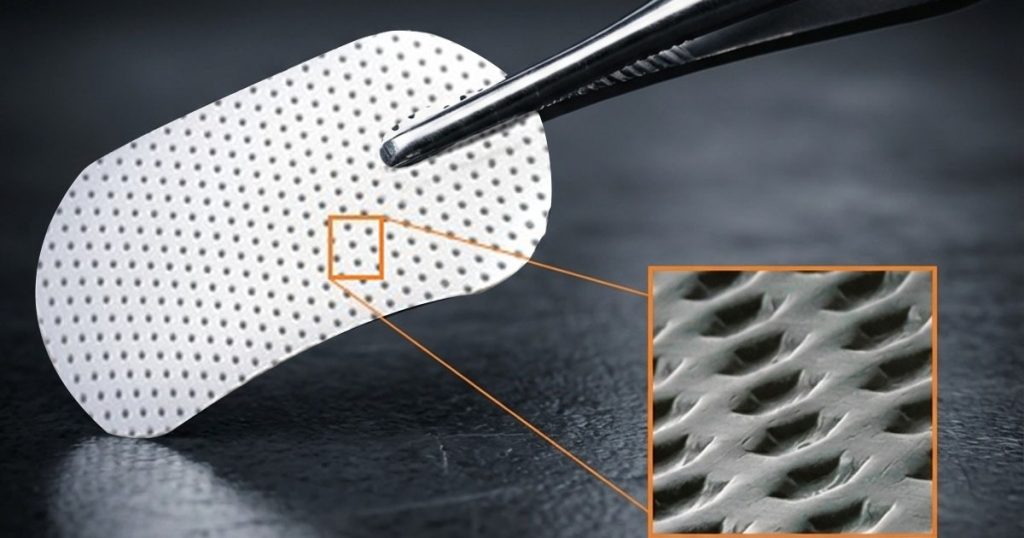
Recommended Product: Xcem Osspore PTFE Membranes
2. Bone Graft Materials
| Graft Type | Properties | Advantages | Challenges |
|---|---|---|---|
| Autograft | Osteogenic, osteoinductive, osteoconductive | Promotes rapid healing and integration | Limited quantity, donorsite morbidity, higher resorption |
| Allograft | Osteoinductive if high quality | No second surgical site | Risk of variable quality and immune reaction |
| Xenograft | Osteoconductive | Excellent space maintenance | Slow resorption, potential for infection |
| Alloplast | Synthetic, osteoconductive | Unlimited supply, low disease risk | Lacks biological activity, slower integration |
| Composite graft | Mix of autograft and xenograft or alloplast | Balances biological activity and volume stability | Requires careful mixing and membrane stabilisation |
3. Membrane Fixation and Stabilization
- Titanium Mesh: Provides additional mechanical support for graft material.
Recommended Product: Xcem Osspore Titanium Membrane
Recent Advances in Guided Bone Regeneration (GBR)
1. Stem Cell Therapy
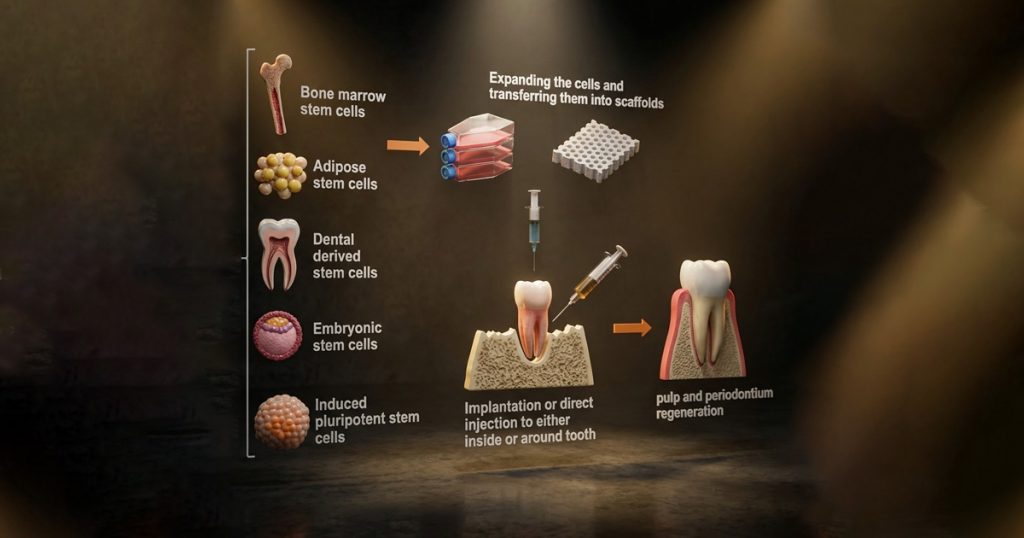
- Scientists are investigating stem cells to regenerate bone and other oral tissues, potentially enabling faster and more effective healing.
2. 3D Printing for Bone Grafts
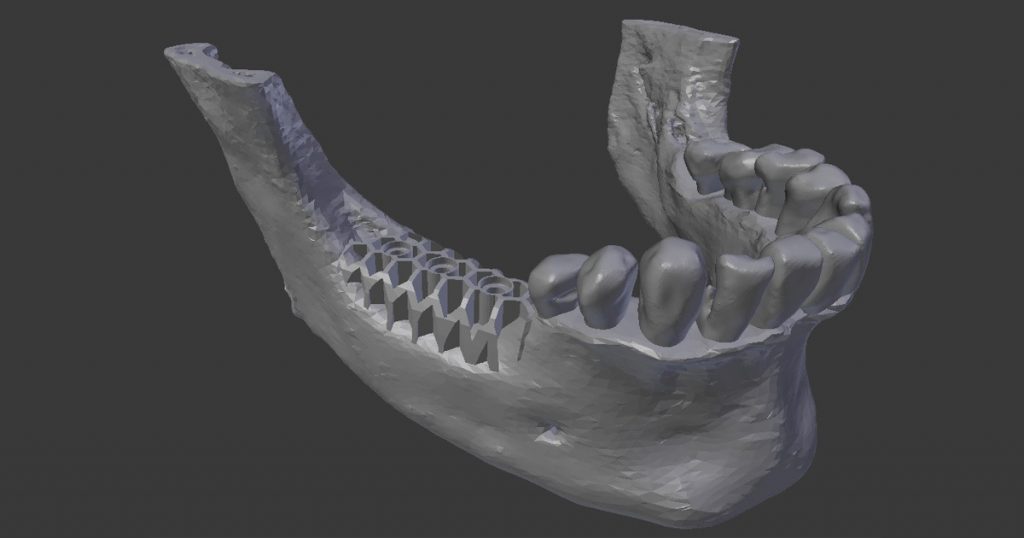
- Clinicians custom-design 3D-printed scaffolds to mimic natural bone structure, promoting bone growth and better integration with existing tissue.
3. Growth Factors and Platelet-Rich Plasma (PRP)
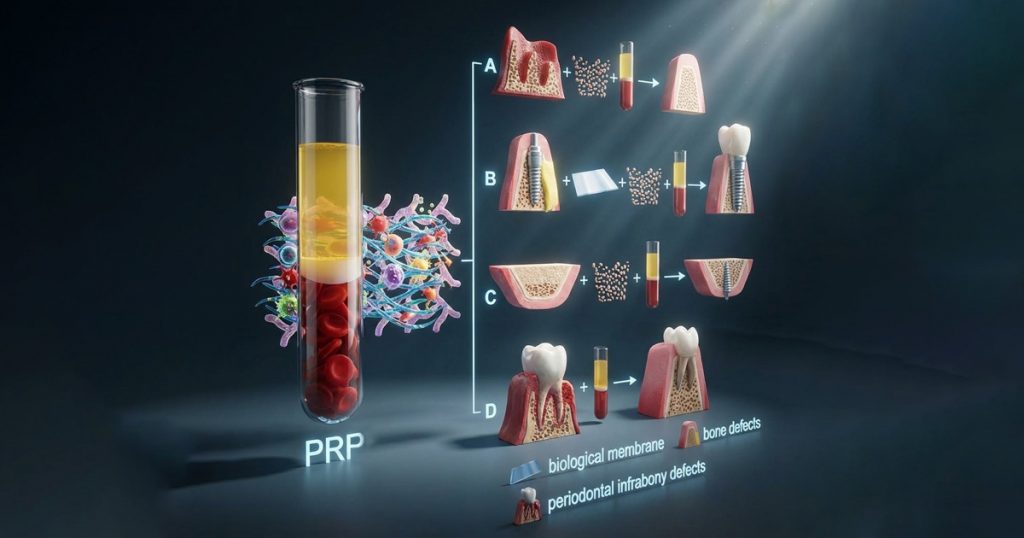
- PRP contains growth factors that accelerate tissue regeneration and enhance bone healing, reducing recovery times and improving outcomes.
4. Laser-Assisted GBR

- Lasers are increasingly being used in GBR procedures to clean the site, remove damaged tissue, and promote healing through precise, minimally invasive techniques.
5. Minimally Invasive GBR

- Pinhole surgical techniques and other less invasive methods are being explored to reduce discomfort and speed up the recovery process.
Conclusion
Guided Bone Regeneration (GBR) is an essential procedure in implant dentistry, offering a solution for patients with insufficient bone for implants. With the right approach, proper techniques, and high-quality products, GBR can restore lost bone and provide a solid foundation for dental implants.
The advances in stem cell therapy, 3D printing, and bioactive materials continue to improve the efficiency of GBR and make the procedure even more reliable. By understanding the indications, contraindications, and the step-by-step process, dental professionals can provide the best possible care for their patients.
FAQ’s
No. Minor defects with intact bony walls and good primary implant stability may heal without GBR. GBR is recommended when defects are large or when bone walls are missing, compromising implant support.
The barrier membrane excludes fast-growing soft tissue cells from the grafted site. This allows slower-growing osteogenic cells to regenerate bone within a protected and stable environment.
Autogenous bone, allografts, xenografts, and synthetic grafts are commonly used. Autogenous bone provides osteogenic potential, while xenografts and synthetics help maintain volume and long-term stability.
PASS stands for Primary closure, Angiogenesis, Space maintenance, and Stability. These principles are critical to ensure predictable bone regeneration and long-term success of the graft.
Healing typically takes 3–6 months for moderate defects. Larger horizontal or vertical augmentations may require 6–9 months or more before implant placement.
Dr. Bhavishya Arora
Author
Related Articles

Self-Etch vs. Selective-Etch vs Total-Etch: A Clinical Decision Guide for Everyday Restorations
IntroductionIn restorative dentistry, bonding success does not depend only on the composite resin or adhesive brand. More often than not, long-term success or f

Tissue-Level vs Bone-Level Implants: Clinical Selection Guide
In modern implantology, the debate isn't about which system is "better," but rather which design is most compatible with the patient’s specific anatomy. Implan

Paediatric Pulp Therapy: Guidelines & Best Materials (Pulpotomy / Pulpectomy)
Introduction to Pediatric Pulp Therapy In children, caries reaches the pulp fast because primary teeth have thinner enamel, dentin and larger pulp chambers.