
Digital Occlusion Analysis: The Future of Bite Correction
Did you ever sacrifice a crown that was perfect on paper but "felt wrong" to the patient? Or struggle with a patient complaining of ache even when your occlusion was concordant with articulating paper? Yes? You're not alone. Bite correction has never been one of dentistry's most difficult areas of practice because even slight imbalances can cause discomfort, fractures, TMJ disorders, or treatment failure.
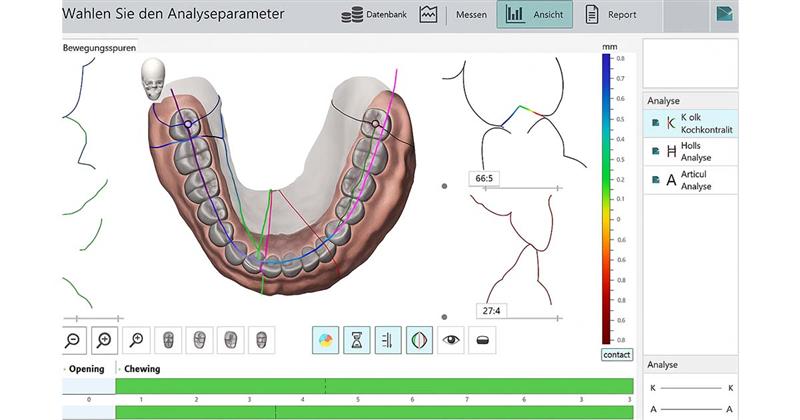
That's where Digital Occlusion Analysis (DOA) steps in. Pressure sensors and computer programs give dentists accurate, live feedback about how teeth contact and distribute force. That means fewer trial-and-error tweaks and more predictable outcomes.
What is Digital Occlusion Analysis?
In a nutshell, Digital Occlusion Analysis is a new technology that replaces "red-blue marks on paper" with precise facts. It tells you:
- When teeth touch (timing of contacts)
- How tightly they contact (distribution of force)
- Which teeth bear extra load
- Left-right symmetry
Instead of attempting to find out which mark is heavier or if the contact is premature, DOA presents unbiased facts that both patients and dentists can see.
Why Traditional Methods Fall Short ?
Articulating paper, wax bites, and shimstock foils have been employed by dentists for decades. They function, but they are insufficient.
| Traditional Method | Limitations |
| Articulating paper | Displays contact points but not force or timing. |
| Wax bites | Can be distorted when removed, decreasing accuracy. |
| Clinical judgment | Is subjective and varies on Dentists. |
The catch? These techniques don't measure occlusion in numbers. A "mark" doesn't indicate whether one molar is taking 40% more force than the other. And that's where digital analysis comes in handy.
How Digital Occlusion Analysis Works ?
The process is simple and easily incorporated into routine practice:
| Step | What Happens | Purpose |
| 1. Sensor Placement | A thin pressure-sensitive sensor (such as a film) is put between the teeth. | To register bite forces. |
| 2. Biting Movements | Patient bites, chews, or moves the jaw as instructed. | Copies true function |
| 3. Data Collection | Force, timing, and occlusal sequence of contacts are sensed with sensors. | Provides accurate bite map. |
| 4. Software Analysis | The results appear in the form of vibrant graphics and 3D structures. | It is simple to interpret. |
| 5. Treatment Planning | Dentist accurately makes adjustments based on data. | Restores comfort & equilibrium. |
The entire test normally takes under 5 minutes and is completely painless.
Benefits of Digital Occlusion Analysis :
Why would a dentist invest in this technology? Because the AI benefits both clinician and patient:
| Benefit | Impact |
| Accuracy | Records exact timing and force of each contact. |
| Better diagnosis | Detects premature contacts and bite imbalances prior to symptoms. |
| Treatment success | Improves outcomes of crowns, bridges, implants, and orthodontic therapy. |
| Patient trust | Patients understand the problem and are more likely to comply with treatment based on visual information. |
| Documentation | Computer records provide medico-legal documentation and progress monitoring. |
| Efficiency | Saves time spent on trial-and-error occlusal adjustments. |
Applications in Contemporary Dentistry
Digital occlusion analysis is no luxury feature. It has functional, everyday applications in dental specialties:
-
Restorative Dentistry
- Avoids new crowns, bridges, and fillings from interfering with bite.
- Avoids post-op hypersensitivity from high points.
-
Implantology
- Avoids overload of implants through management of occlusal forces.
- Essential since implants lack the periodontal ligament and therefore cannot adjust themselves.
-
Orthodontics
- Preserves bite during aligner or braces treatment.
- Provides balanced occlusion at the end of treatment.
-
Prosthodontics
- Helps in the production of natural dentures and prosthetic devices.
-
TMJ & Orofacial Pain
- Detects imbalances that can lead to strain and pain in the joints.
- Help in the management of chronic pain cases by transferring forces.
Traditional vs. Digital Occlusion
| Aspect | Traditional Occlusion | Digital Occlusion Analysis |
| Accuracy | Visual & subjective | Objective, measurable, data-driven |
| Contact detection | Points only | Timing, force, sequence, balance |
| Reproducibility | Varies between dentists | Consistent and repeatable results |
| Patient engagement | Limited | Visual reports enhance patient awareness |
| Treatment tracking | Manual check-ups | Time-based digital tracking |
Patient Experience with DOA
The greatest undervalued advantage is patient education. Most patients struggle to understand what "high spots" are. When they see a 3D representation of one tooth taking 40% of the bite load, they instantly realize why adjustment is needed.
This open book creates trust and increases treatment acceptance.
Challenges and Considerations
As with any technology, DOA has considerations:
- Equipment cost – Sensors and software are a one-time investment.
- Learning curve – Dentists must learn to interpret graphs and data.
- Integration – Best when utilized within a comprehensive digital workflows (CAD/CAM, digital impressions).
But once adopted, it rewards with reduced chairtime, remakes, and unhappy patients.
Fun Facts About Occlusion
- Every swallow takes only 0.2 seconds, but your teeth come together as many as 700 times a day!
- A 50-micron high filling can misalign a bite.
- Digital occlusion sensors are capable of detecting differences of only 8 microns.
- Equilibrated occlusion not only reduces dental wear but also headaches and muscle pain in the majority of patients.
The Future of Bite Correction
As dentistry becomes more digital, occlusion analysis will play an increasingly important role. The future trends may include:
- Bite adjustment recommendations based on artificial intelligence.
- Aligner software integration to treat predictively.
- Wearable trackers of occlusion to monitor forces during everyday chewing.
This means less remake, less complaint, and happier patient.

Conclusion
Digital Occlusion Analysis is no longer just a “nice-to-have.” It’s a game-changer in modern dentistry. By providing measurable, reproducible, and easy-to-understand data, it bridges the gap between what dentists see and what patients feel.
Whether you’re adjusting a single filling, delivering implants, or finishing an orthodontic case, DOA ensures your treatment is precise, predictable, and patient-approved.
The future of bite correction is here and it’s digital.
FAQs
Q1. Is digital occlusion analysis painful?
Not at all. The sensor is very thin and patient friendly.
Q2. Can it replace articulating paper?
Not a replacement, but a complement. Paper shows where contacts are, whereas DOA shows when and how hard.
Q3. How long does it take?
Less than 5 minutes in most cases.
Q4. Is it useful only for specialists?
No, general practitioners also benefit just as much, especially for restorative treatments.
Q5. Does it add to patient expense?
A few clinics charge a small fee, but most patients consider it worth it for long-term comfort.
Q6. Can DOA prevent implant failure?
Yes. By leveling forces, it protects implants from fracture and overload.
Dr. Noopur Aggarwal
Author
Related Articles

Self-Etch vs. Selective-Etch vs Total-Etch: A Clinical Decision Guide for Everyday Restorations
IntroductionIn restorative dentistry, bonding success does not depend only on the composite resin or adhesive brand. More often than not, long-term success or f

Tissue-Level vs Bone-Level Implants: Clinical Selection Guide
In modern implantology, the debate isn't about which system is "better," but rather which design is most compatible with the patient’s specific anatomy. Implan

Paediatric Pulp Therapy: Guidelines & Best Materials (Pulpotomy / Pulpectomy)
Introduction to Pediatric Pulp Therapy In children, caries reaches the pulp fast because primary teeth have thinner enamel, dentin and larger pulp chambers.