
Composite Failures: Causes, Prevention & Clinical Solutions
Composite restorations remain the most common direct treatment in dentistry-yet they are also among the most technique-sensitive. Composite Failures often occur not because of the material but due to small deviations in bonding, moisture control, preparation design, or occlusal planning. Understanding these hidden factors helps clinicians achieve predictable, long-lasting restorations.
Why Composite Restorations Fail
1. Improper Isolation and Moisture Contamination

Even minor contamination from saliva, blood, or crevicular fluid disrupts the adhesive layer.
- High-risk situations: cervical lesions, deep proximal boxes, inflamed gingiva.
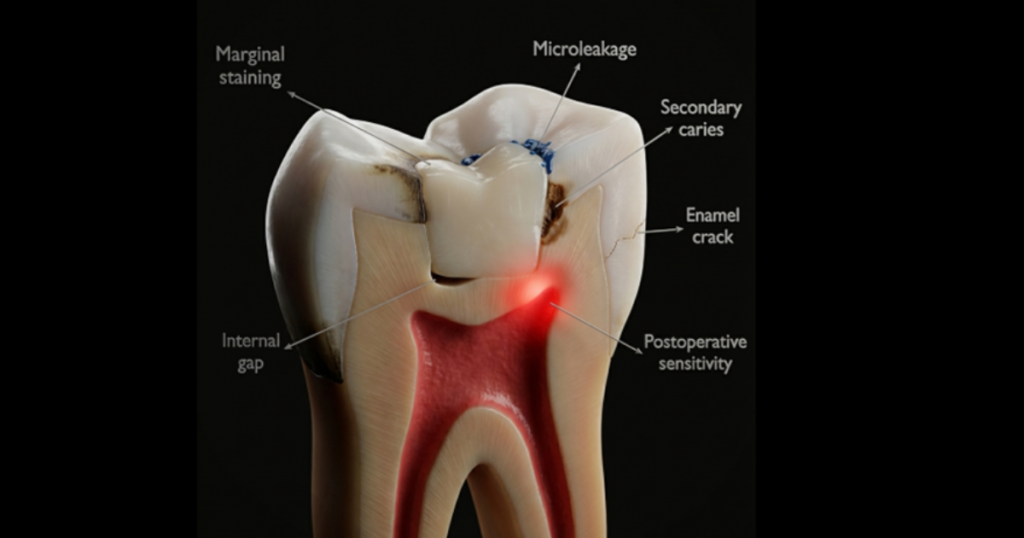
- Consequence: microleakage → sensitivity → marginal discoloration → secondary caries.
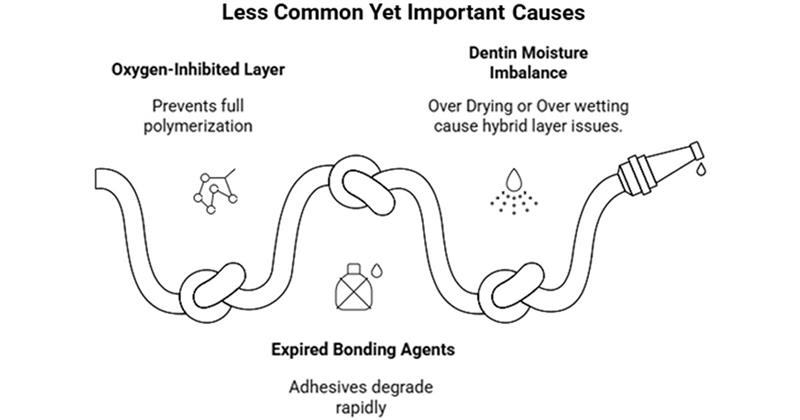
2. Over-Curing or Under-Curing the Adhesive Layer

Curing errors are responsible for many early failures:
- Insufficient irradiance → weak hybrid layer
- Excessive curing distance → low conversion
- Thick adhesive pools → flexible, weak base
Result: debonding, postoperative pain, and fracture at the adhesive–dentin interface.
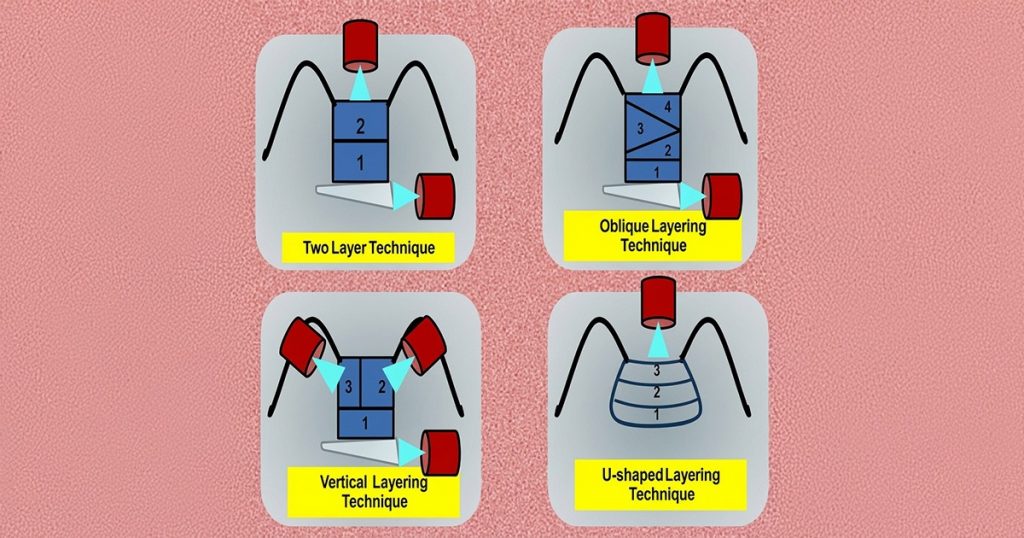
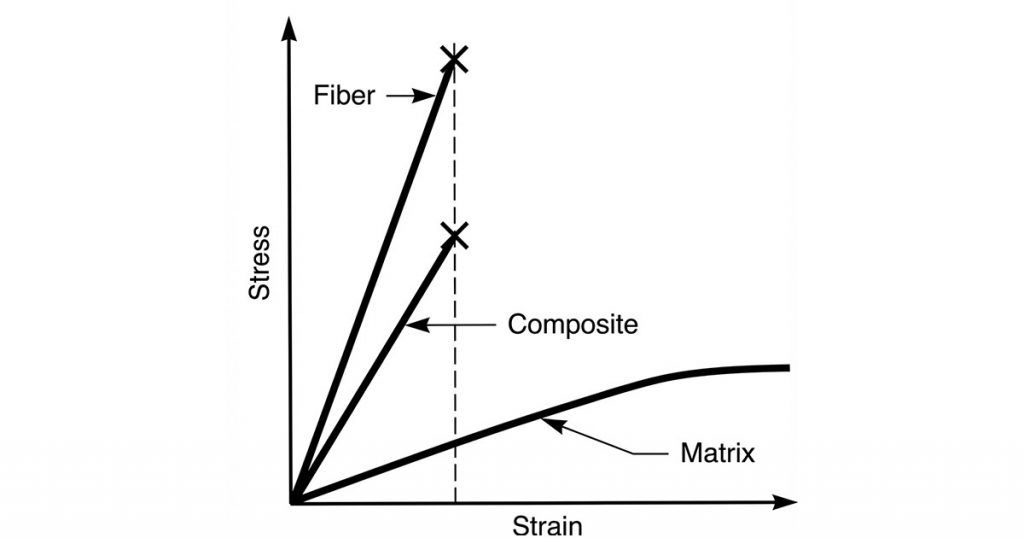
3. Incorrect Layering Technique and Polymerization Stress
Composite shrinkage creates internal stress that exceeds bond strength.
- High-stress scenarios: bulk fills in thin-walled cavities, C-factor heavy preps.
- Common outcomes: cusp deflection, microcracks, marginal gaps.
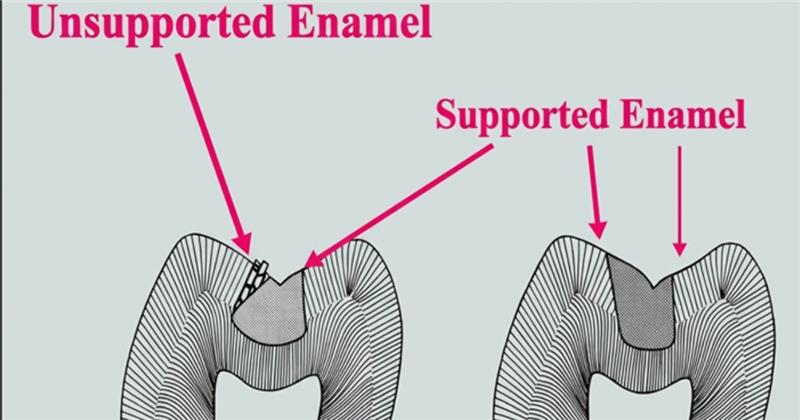
4. Poor Cavity Design and Unsupported Enamel
Sharp internal line angles and unsupported enamel increase fracture risk.
- Typical failures: chipping at margins, proximal fracture lines, “ditching” at gingival margins of Class II restorations.
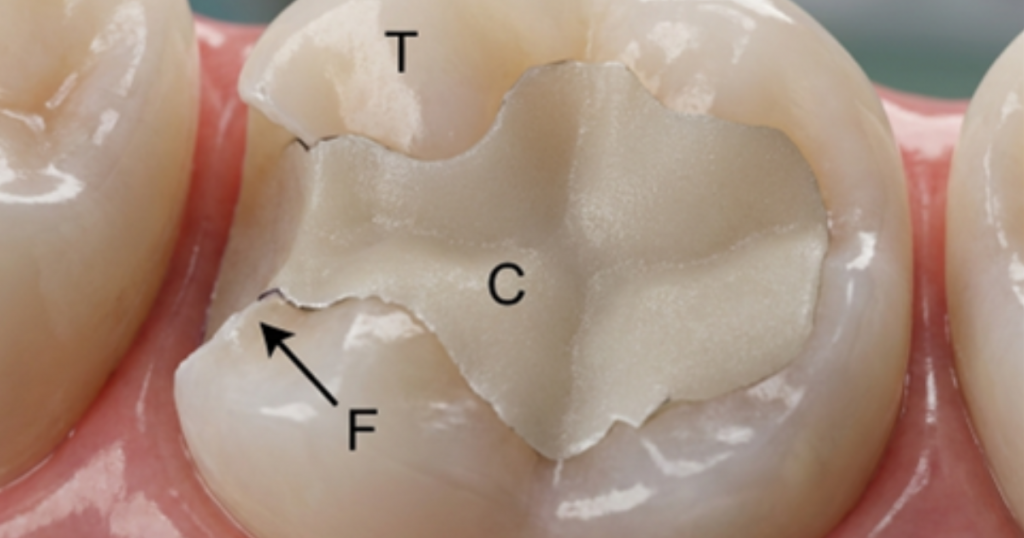

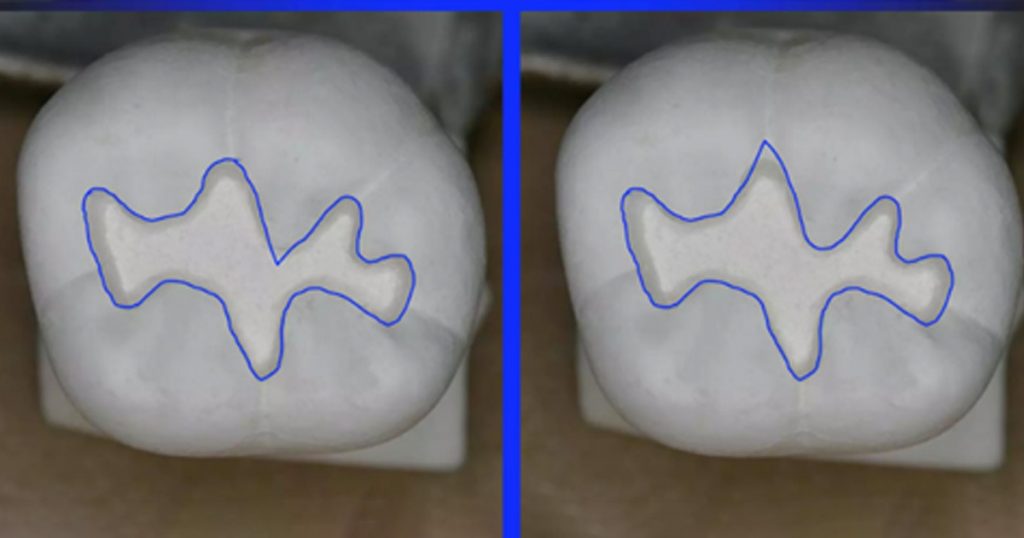
Fracture of the marginal ridge of a composite class II restoration in a posterior molar in a clinical setting ( C 1⁄4 composite , T 1⁄4 tooth substance, F 1⁄4 fracture)
5. Occlusal Mismanagement
Heavy occlusal load is a major, often underestimated, cause.
- Risk zones: functional cusps, high-stress contact points.
- Signs of failure: composite wear, fracture lines, open margins, repeated chipping.
6. Inadequate Adhesive Protocol Choice (Etch-and-Rinse vs Self-Etch)
Not all adhesives behave the same.
Examples:
- Over-etching dentin → sensitivity + weak hybrid layer
- Incompatibility between universal adhesives and self- or dual-cure materials

How to Prevent Composite Failures (Technique-Based Protocols)
1. Prioritize Isolation (Rubber Dam or Alternative Barriers)
Isolation failures are one of the biggest predictors of long-term breakdown.
Use Teflon tape, wedges, retraction cords, matrix systems, or hemostatic agents as needed.

Products- Waldent FlexiShield Rubber Dam Sheets (Sanctuary), Waldent Rubber Dam Kit of 21 (K16/2)
2. Follow a Strict Bonding Protocol
- Perform selective enamel etching for best enamel seal

Product- Waldent BESTEtch
- Ensure adequate light intensity (≥1000 mW/cm²)
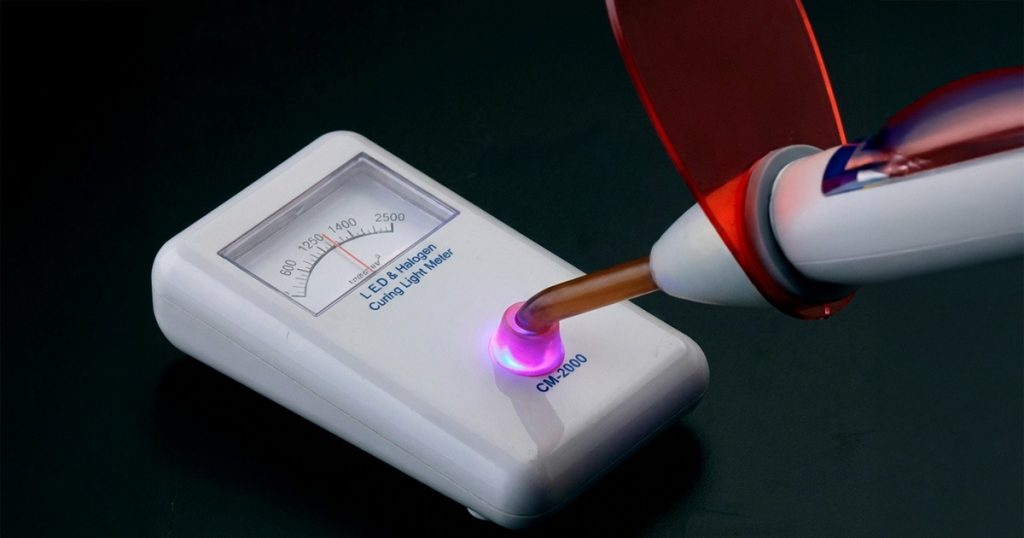
- Maintain curing tip 0–5 mm from the surface

- Consider incremental warm composite placement for better adaptation and lower stress
Product- Waldent NanoFill Zirconium Composite Kit
3. Manage Polymerization Shrinkage
- Use oblique or centripetal layering
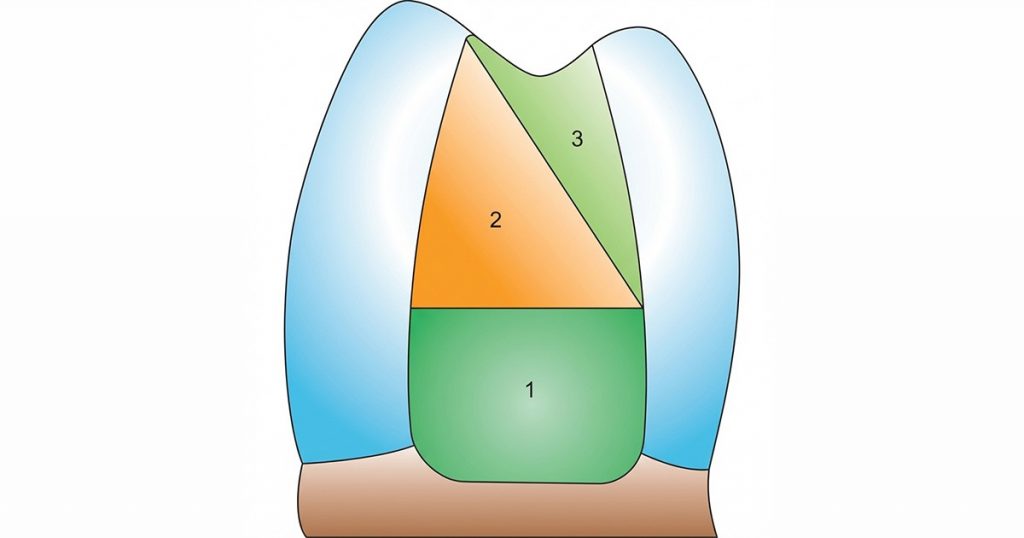
- Consider low-shrink or stress-relieving composites
- For deep cavities, preheat composite for better flow and reduced voids

Product- Endoking Nanowarm Composite Warmer
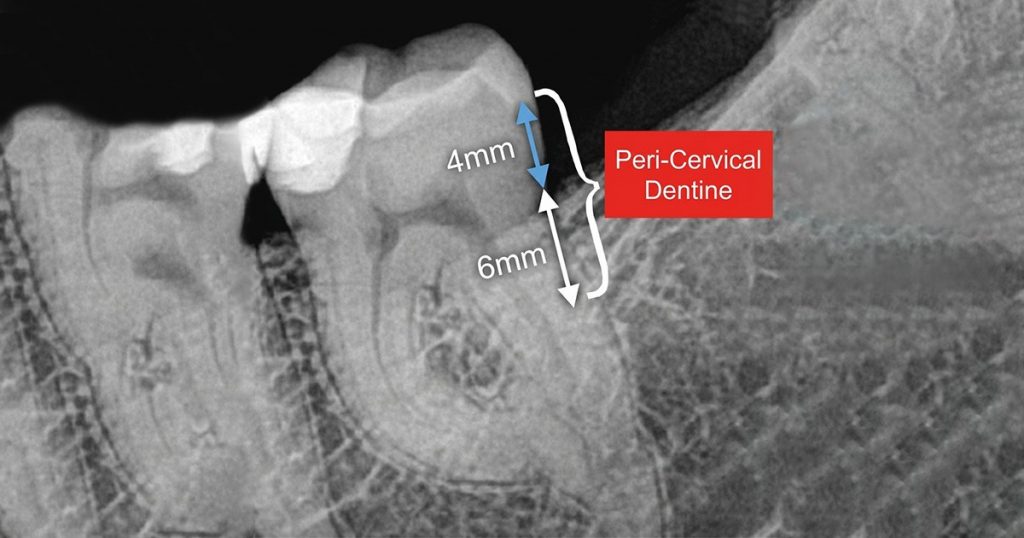
4. Respect Biomechanics
- Preserve pericervical dentin
- Reduce internal line angles
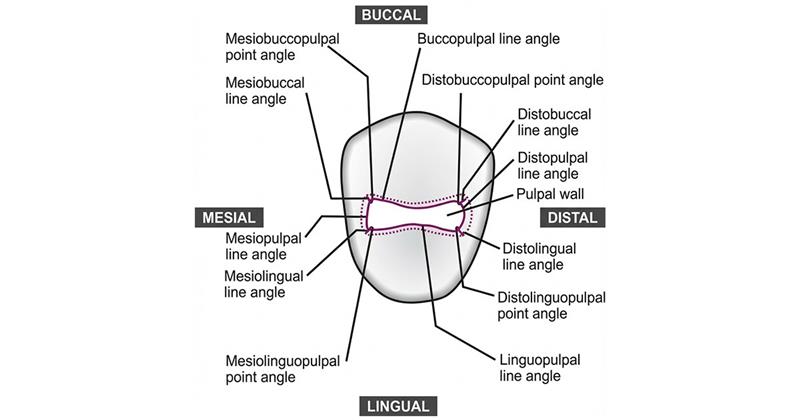
- Round all cavosurface margins
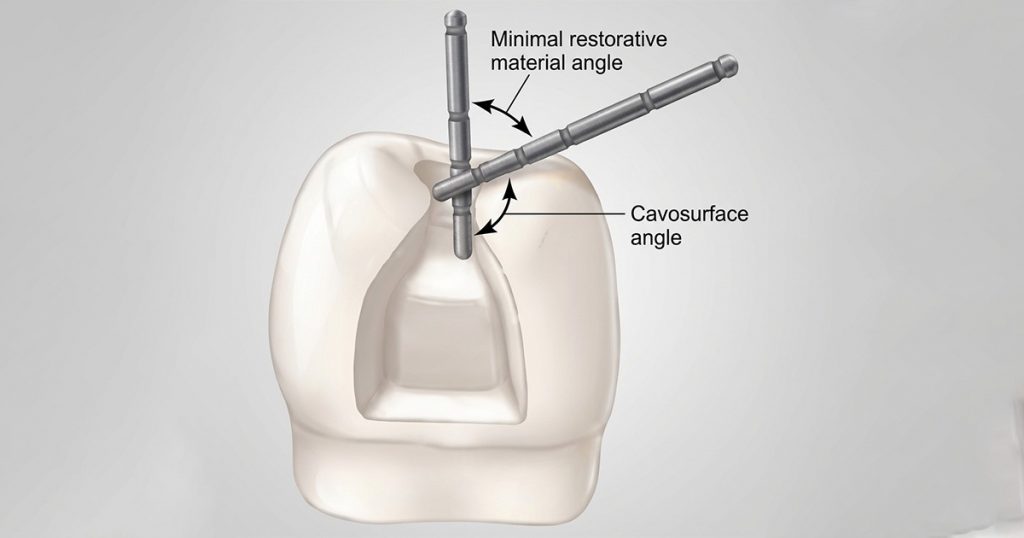
- Avoid sharp transitions that become fracture points
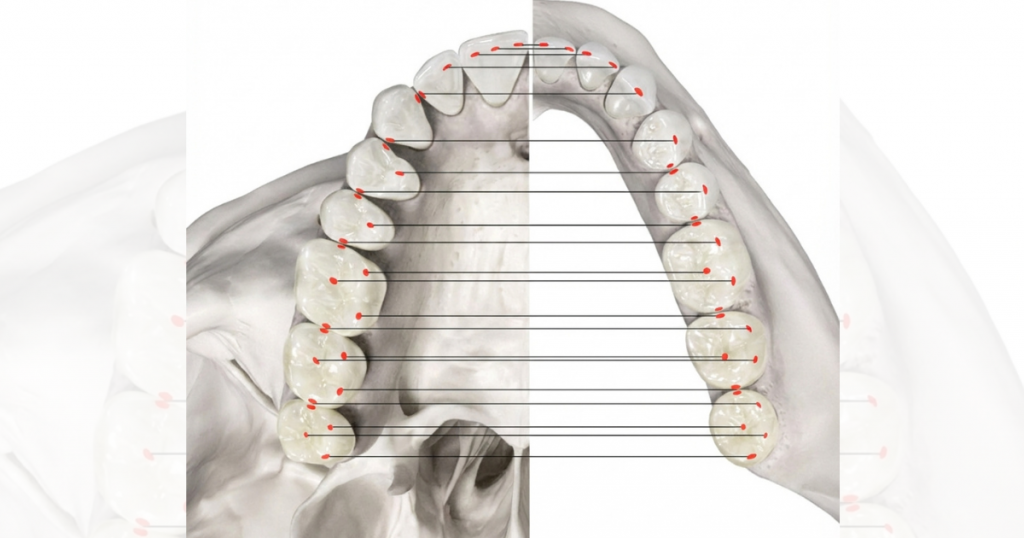
5. Occlusal Planning: A Critical, Often Missed Step
- Verify functional pathways: protrusion, lateral, working vs nonworking
- Keep composite out of heavy centric stops whenever possible
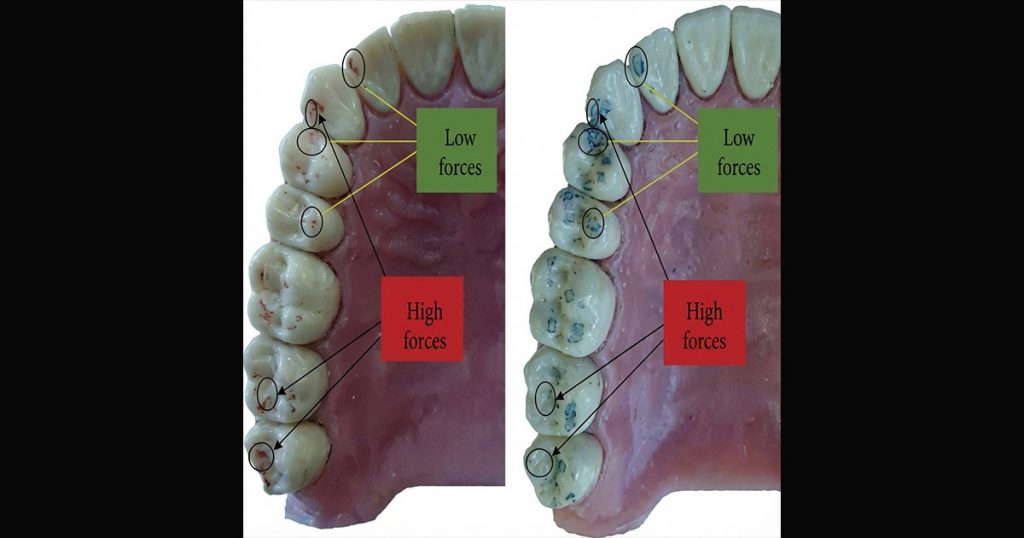
- For bruxers: use higher-strength materials or consider indirect option

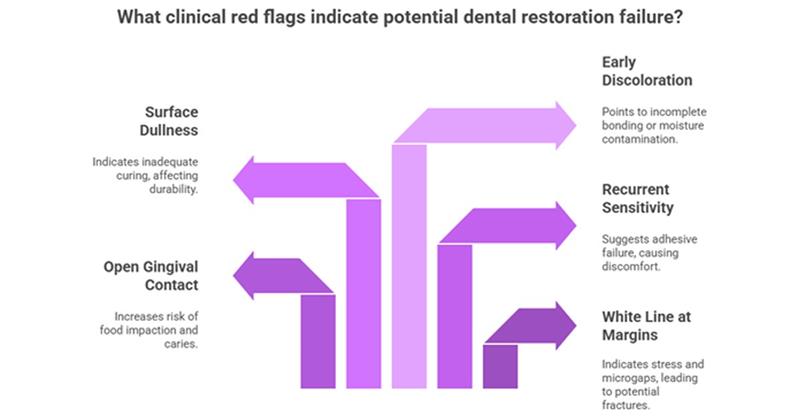
Clinical Red Flags That Predict Early Composite Restoration Failure
Best Practices for Long-Lasting Composite Restorations
1. Use High-Output, Calibrated Light-Curing Units
Regularly check irradiance; replace aging tips.
Product- Waldent M Cure 10 Light Cure Unit, Waldent ECO Plus Light Curing Unit
2. Control Contact & Contour
Use sectional matrices, rings, and anatomically shaped wedges for predictable proximal form.
Products- Tor Vm Transparent Sectional Contoured Matrices, Tor Vm Sectional Contoured Metal Matrices - Universal Kit No.1.398
3. Finishing & Polishing Protocols
Smooth margins reduce plaque retention and staining.
Multi-step polishing systems improve longevity significantly.
Products- Youdent Composite Polishing Kit Pink RA, SuperEndo Composite & Porcelain Finishing Bur Kit
4. Regular Follow-Up and Maintenance
Teach patients to avoid excessive load and monitor restorations during recalls.
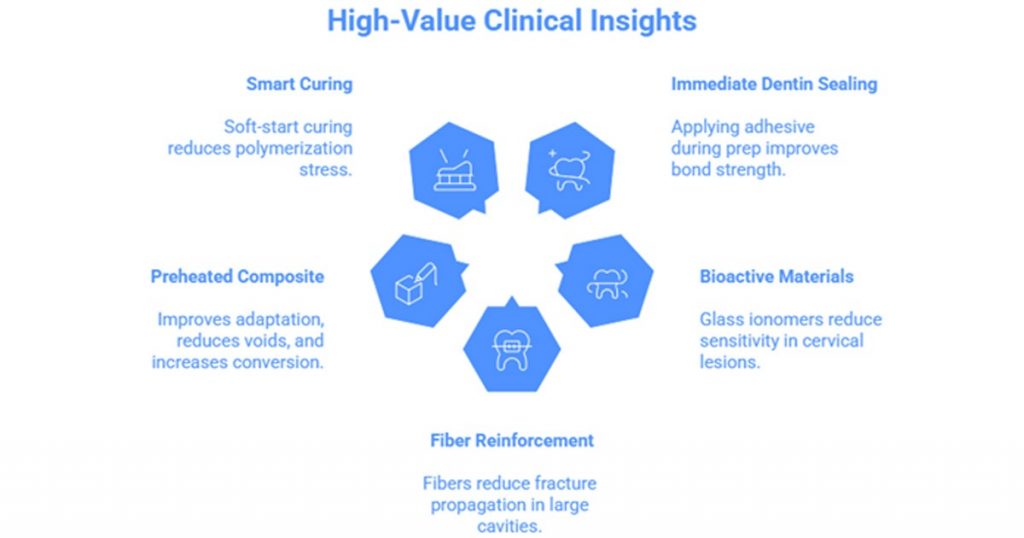
Advanced Composite Longevity Tips (High-Value Clinical Insights)
Conclusion
Composite longevity is determined far more by clinical technique than by the material itself. When isolation is meticulously maintained, bonding protocols are followed precisely, and layering is performed in a way that minimizes polymerization stress, the restoration’s predictability increases significantly. Incorporating thoughtful occlusal planning, sound biomechanical principles, and proper curing practices further strengthens long-term outcomes. With these components executed consistently, composite restorations can deliver durable function, reliable esthetics, and high patient satisfaction.
FAQ's
Composite failures usually result from technique-sensitive errors such as inadequate isolation, improper curing, poor bonding protocol, polymerization stress, or mismanaged occlusion. Material quality matters, but long-term success depends primarily on clinical execution.
Even tiny amounts of saliva, blood, or crevicular fluid disrupt the adhesive layer. This causes microleakage, postoperative sensitivity, marginal staining, and eventually secondary caries-making isolation one of the strongest predictors of longevity.
Under-curing leads to a weak hybrid layer and poor bond strength.
Over-curing, especially when the adhesive pools, creates a flexible, unstable base. Both scenarios increase the risk of debonding and fracture at the adhesive-dentin interface.
As composite shrinks during curing, it pulls away from cavity walls, creating internal stress. If this stress exceeds bond strength, it results in cusp deflection, marginal gaps, microcracks, and early restoration breakdown.
Dr. Yashasvi Sharma
Author
Related Articles

Self-Etch vs. Selective-Etch vs Total-Etch: A Clinical Decision Guide for Everyday Restorations
IntroductionIn restorative dentistry, bonding success does not depend only on the composite resin or adhesive brand. More often than not, long-term success or f

Tissue-Level vs Bone-Level Implants: Clinical Selection Guide
In modern implantology, the debate isn't about which system is "better," but rather which design is most compatible with the patient’s specific anatomy. Implan

Paediatric Pulp Therapy: Guidelines & Best Materials (Pulpotomy / Pulpectomy)
Introduction to Pediatric Pulp Therapy In children, caries reaches the pulp fast because primary teeth have thinner enamel, dentin and larger pulp chambers.