Autoclave Sterilization Guide: Ensuring Safety and Efficiency

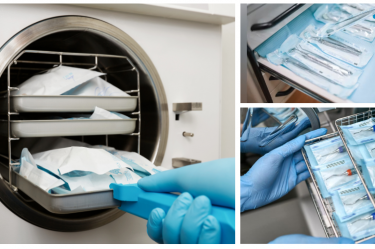
Dental clinics, like hospitals, can become a hub of contaminants if proper sterilization and hygiene methods are not followed. This can pose a risk of infections to both patients and dental professionals working in such environments. To prevent cross-contamination and the spread of diseases, it is important that the dental equipment and instruments used are thoroughly sterilized. An autoclave is one such dental equipment that is a must-have for a dentist’s clinical setup for proper sterilization.
In this blog, we will discuss what an autoclave is, its working principle, its components, the appropriate sterilization cycles, and the types of instruments, glassware, plasticware, and other materials that can be sterilized using it. Additionally, we will share cleaning and maintenance tips to ensure the efficient functioning of an autoclave.
What is an Autoclave?
An autoclave, also known as a steam sterilizer, is a machine that uses pressurized steam as a physical method of sterilization to disinfect equipment and supplies in medical and laboratory settings. Autoclave steam is capable of killing bacteria, viruses, fungi, and even the spores on the equipment that are introduced into the steam chamber.
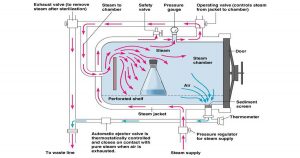
Working principle of an Autoclave
The working principle of autoclave includes steam above 100°C or saturated steam since it has a better killing power than dry heat. Bacteria are more susceptible to moist heat as bacterial protein coagulates rapidly. Saturated steam can penetrate porous material easily. When steam comes into contact with a cooler surface it condenses to water and liberates its latent heat to that surface, for example, 1600ml of steam at 100°C and atmospheric pressure condenses into 1ml of water at 100°C and releases 518 calories of heat.
The large reduction in volume sucks in more steam to the same site and the process continues till the temperature of the article is raised to that of the steam. The condensed water produces moist conditions for killing the microbes present.
Components of an Autoclave: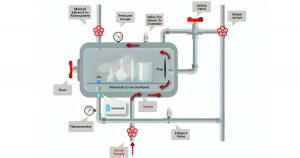
An autoclave is a high-pressure sterilization device, functioning similarly to a modified pressure cooker or boiler. It consists of a vertical and horizontal cylinder of gunmetal or stainless steel in a supporting iron case. The lid is fastened by screw clamps and rendered air-tight by an asbestos washer. The lid bears a discharge tap for air and steam, a pressure gauge, and a safety valve. Heating is generally done by electricity. The steam circulates within the jacket and is supplied under high pressure to the inner chamber where materials are kept for sterilization.
Procedure:
The process of operating an autoclave involves several sequential steps to ensure effective sterilization. The cylinder is first filled with sufficient water and the material to be sterilized is placed on the tray. The lid is then closed with the discharge tap open. The heater is put on. The safety valve is adjusted to the required pressure. After boiling of water, the steam and air mixture is allowed to escape till all the air has been displaced.
This can be tested by leading the escape steam-air mixture into a pail of water through rubber tubing. When the air bubble stops coming in the pail it indicates that all the air has been displaced. The discharge tap is now closed. The steam pressure rises inside and when it reaches the desired set level of 15 pounds (lbs) per square inch, the safety valve opens, and the excess steam escapes. From this point, the holding period (15 minutes) is counted.
After the holding period, the heating is stopped and the autoclave is allowed to cool till the pressure gauge indicates that the pressure inside is equal to the atmospheric pressure. The discharge tap is opened slowly and air is allowed to enter the autoclave. The lid is now opened and the sterilized material is removed.
Sterilization conditions:
Temperature – 121°C
Chamber pressure – 15 pounds (lbs) per square inch
Holding time – 15 minutes
These conditions are generally used, however, sterilization can also be done at higher temperatures, at 126°C (20 lbs/square inch) for 10 minutes or at 133°C (30 lbs/square inch) for 3 minutes.
Uses:
- To sterilize culture media, rubber material, gowns, dressing, gloves, etc.
- It is particularly useful for materials that cannot withstand the higher temperature of a hot air oven.
iii. For all glass syringes, a hot air oven is a better sterilizing method.
Autoclave Compatible and Incompatible Material
Compatible materials:
- Biological cultures and stocks
- Culture dishes and related materials
- Contaminated solid items like pipette tips, Petri dishes, etc.
- Discarded live (including attenuated) viruses/ vaccines
- Polycarbonate(pc) and propylene (pp) plastics
- Borosilicate glass
- Stainless steel instruments like scalers, burs, pliers, forceps etc.
Incompatible Materials:
- Materials containing solvents, volatile or corrosive, or flammable chemicals
- Material contaminated with chemotherapeutic agents or cytotoxic drugs
- Material containing Bleach (Neutralize waste containing bleach with equal amounts of 1% sodium thiosulfate in water before autoclaving)
- Carcinogens or mutagens (i.e. ethidium bromide)
- Phenol and Trizol
- Polystyrene (PS), polyethylene (PE), and high-density polyethylene (HDPE) plastics
- Household glassware
Precautions:
- The air must be allowed to escape from the chamber as the temperature of air- steam mixture is lower than that of pure steam.
- Materials should be arranged in such a manner as to ensure free circulation of steam inside the chamber.

Cleaning and maintaining autoclaves
- Use autoclave cleaners: Autoclave cleaners are specifically formulated to remove hard water deposits from them. Usage of other chemicals to remove these precipitates can harm the autoclave sterilizer.
- Use distilled water only: Usage of distilled water in autoclaves ensures the removal of impurities and contaminants including bacteria, particles, dissolved solids, etc. helping to provide the cleanest water possible. This eventually helps in preventing minerals from corroding the autoclave, prolonging the life.
- Cleaning: The cleaning of the heating element should be done daily and the water reservoir should be drained weekly. Whereas, the inspection of the wiring and safety valves should be done every month. Inspection of the entire autoclave should be done quarterly or annually without any delay.
- Other than the above-mentioned, the manufacturer’s instructions should be followed for proper maintenance of the machine.
Read Also: Types of Autoclaves: A Complete Guide for Dental Practice
Conclusion:
Autoclaves play a critical role in ensuring the sterilization of dental instruments, glassware, biological cultures, and many other everyday dental supplies, thereby maintaining a safe and hygienic clinical environment. Their ability to eliminate even the most resilient microorganisms makes them an essential dental equipment in every clinical setup. Proper understanding of their functionality, sterilization conditions, and maintenance not only enhances their performance but also extends their lifespan.
By prioritizing proper autoclave usage and upkeep, dental professionals can ensure the highest standards of infection control, protecting both patients and staff from potential health risks. This commitment to hygiene and safety builds trust and confidence in your practice, reinforcing the importance of sterilization as a cornerstone of quality dental care.
For a wide range of reliable and efficient autoclaves, visit DentalKart, the best online dental store, and take the next step toward achieving a safer clinical environment.
Frequently Asked Questions:
What is the use of autoclave in dentistry?
An autoclave is used in dentistry to sterilize dental instruments and equipment, ensuring they are free from harmful microorganisms, including bacteria, viruses, fungi, and spores. This process helps prevent cross-contamination and maintains a safe and hygienic clinical environment for both patients and dental professionals.
What dental instruments can be autoclaved?
A wide range of medical and dental instruments and supplies can be autoclaved; these include some of the following:
- Biological cultures and stocks
- Culture dishes and related materials
- Contaminated solid items like pipette tips and Petri dishes
- Polycarbonate (PC) and polypropylene (PP) plastics
- Borosilicate glass
- Stainless steel instruments such as scalers, forceps, and pliers
Instruments made of materials like polystyrene, polyethylene, or household glassware should not be autoclaved, as they are incompatible with the process.
What is autoclave temperature?
The standard sterilization temperature for autoclaves is 121°C at 15 pounds per square inch (psi) pressure for 15 minutes. Alternatively, sterilization can also be done at higher temperatures, such as:
- 126°C at 20 psi for 10 minutes
- 133°C at 30 psi for 10 minutes or even 3 minutes for faster cycles
Does autoclaving destroy bacteria?
Yes, autoclaving is highly effective in destroying bacteria, including their spores. The pressurized steam penetrates porous materials and denatures bacterial proteins, ensuring complete sterilization. It is one of the most reliable methods for eliminating pathogens and maintaining sterile conditions in a dental clinic.
Reference: Textbook of Microbiology, C.P Baveja

No Comment