Tissue-Level vs Bone-Level Implants: Clinical Selection Guide
In modern implantology, the debate isn’t about which system is “better,” but rather which design is most compatible with the patient’s specific anatomy. Implant positioning dictates everything-from how the bone reacts in the first six months to how easily the patient can clean the restoration ten years later.
To achieve long-term success, we must understand the fundamental divide between Tissue-Level (TL) and Bone-Level (BL) philosophies.
Products: Bone level Implant: Apex Konnect Dental Implants 5.0mm
Tissue Level Implant: Xcem XVT Tissue Level Dental Implant
Fundamental Design Differences
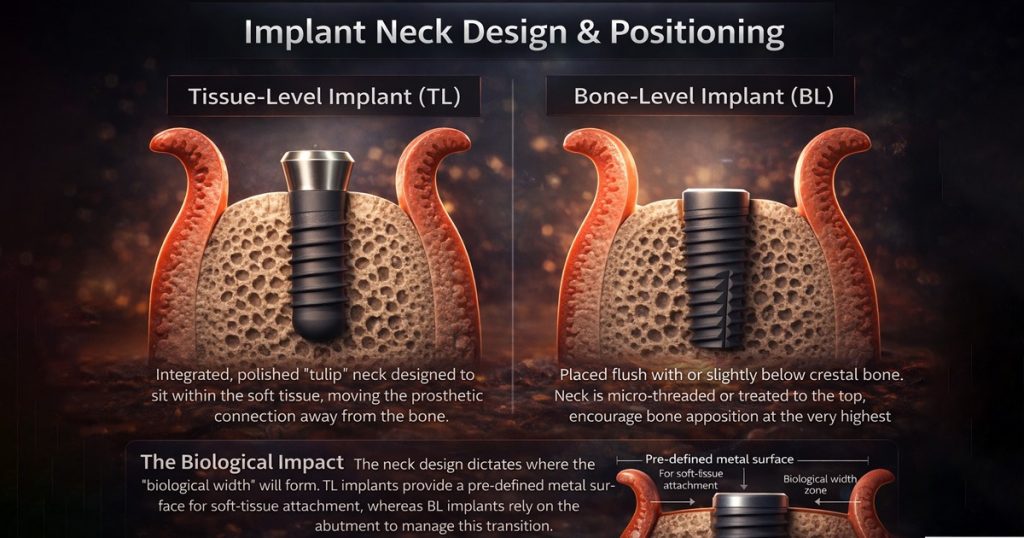
1. Implant Neck Design & Positioning
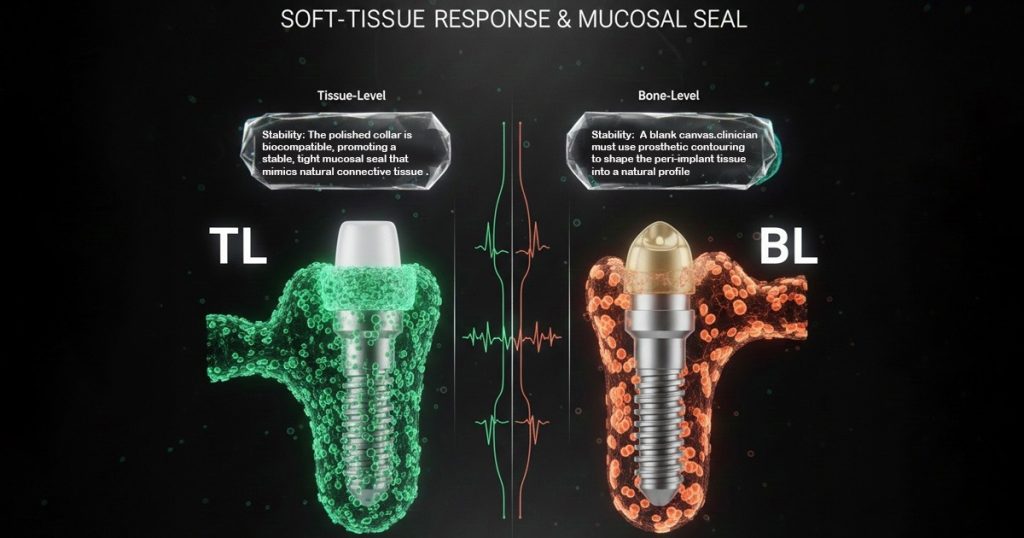
2. Soft-Tissue Response & Mucosal Seal
Clinical Protocol Differences
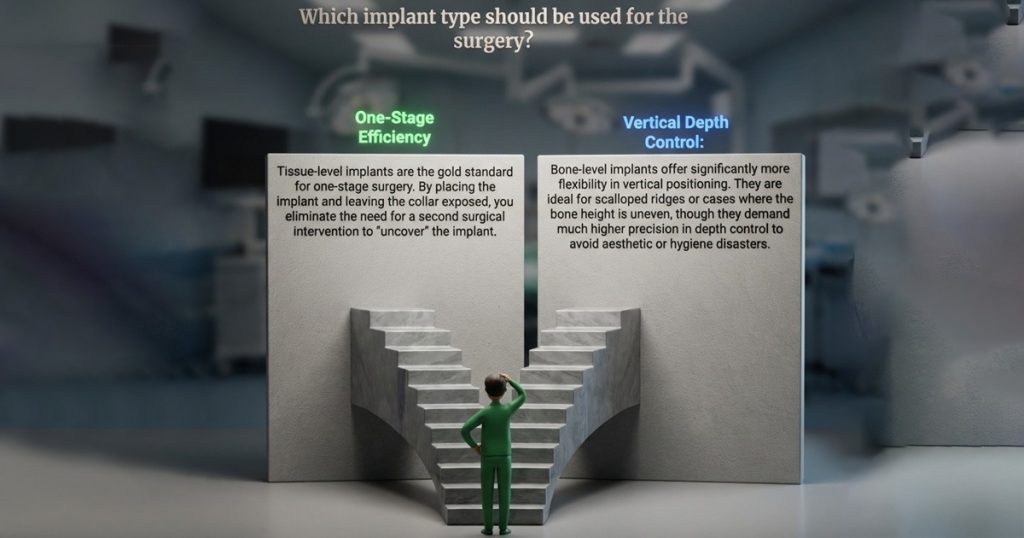
I. Surgical Protocol Considerations
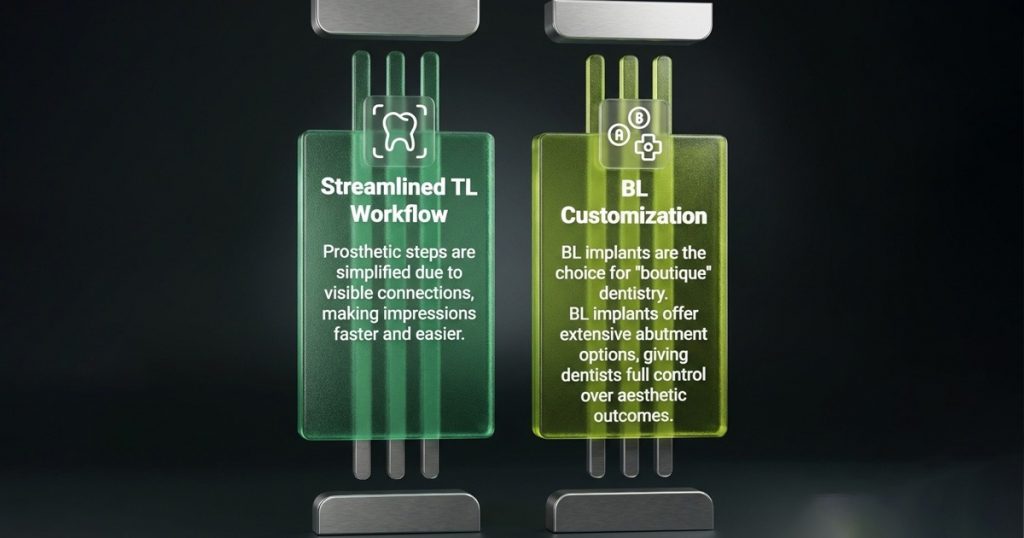
II. Prosthetic Workflow & Restorative Flexibility
III. Maintenance & Long-Term Management

Advantages in Daily Clinical Practice

How to Choose: Structured Clinical Decision-Making
| Clinical Parameter | Tissue-Level Implants | Bone-Level Implants |
| Site Location | Posterior; esthetics are secondary | Anterior; high esthetic demand |
| Soft-Tissue Thickness | Best for thin/moderate biotypes | Preferable for thick biotypes |
| Crestal Bone Priority | Highest (Interface away from bone) | Requires precise “platform switching” |
| Esthetic Requirements | Limited by fixed collar height | Highly customizable emergence |
| Vertical Placement | More forgiving; depth is pre-set | Technique-sensitive; depth is critical |
| Prosthetic Flexibility | Limited abutment modifications | High flexibility in design/angulation |
| Surgical Complexity | Ideal for simple, one-stage cases | Best for staged, complex restorations |
| Hygiene Access | Easier plaque control (Supragingival) | Requires meticulous patient hygiene |
| Peri-Implantitis Risk | Lower interface-related risk | Higher dependence on tissue stability |
| Multi-Unit Cases | Less common (Parallelism issues) | Better for alignment and path of insertion |
Conclusion
The “Hybrid” clinician understands that both systems are essential tools. Tissue-level implants prioritize biological stability and simplicity, making them the workhorse of the posterior arch. Bone-level implants prioritize prosthetic flexibility and aesthetic control, making them indispensable for the “smile zone” and complex reconstructions.
The site’s anatomy, the patient’s ability to maintain hygiene, and the final restorative goal should ultimately dictate your choice.
FAQ’s
The choice depends on patient-specific anatomy, site location, and long-term maintenance needs. Each design serves a different biological and prosthetic purpose, making them complementary tools rather than competing systems.
Implant positioning determines where the biological width forms, how bone reacts during early healing, and how easily the restoration can be maintained over time, directly impacting both stability and hygiene.
Tissue-level implants have an integrated polished collar positioned in soft tissue, while bone-level implants are placed at or below the crestal bone, relying on the abutment to manage the soft-tissue transition.
Every implant connection has a microscopic gap. When this interface is positioned away from the bone, as in tissue-level implants, the risk of inflammatory bone remodeling is significantly reduced.
Their polished collar is highly biocompatible and supports a stable mucosal seal, closely mimicking natural connective tissue attachment and protecting the crestal bone from bacterial micro-movement.



No Comment