The Ultimate Dentist’s Guide to Surgical Periodontal Therapy

Introduction
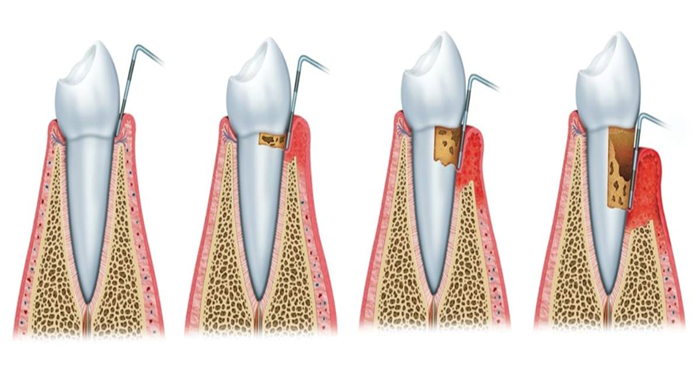
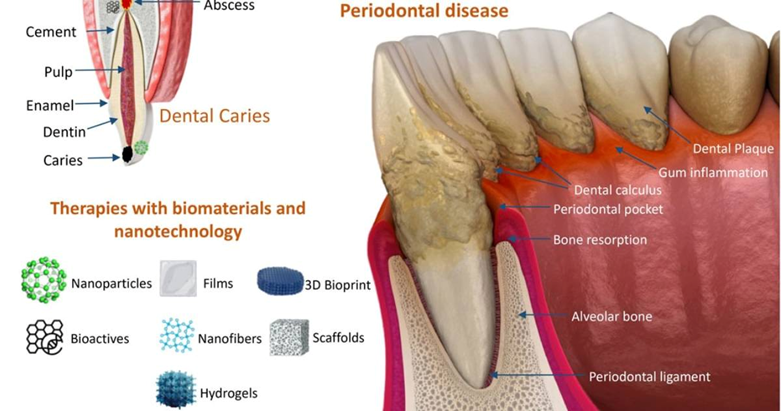
Periodontal disease continues to be one of the most common conditions that come across many dentists. Many patients respond well to scaling and root planning, but some progress to deeper pockets, bone loss, and persistent inflammation. In such cases, surgical periodontal therapy becomes essential.
The good news: Modern periodontal surgery in 2025 is far more precise, minimally invasive, and patient friendly. This guide gives dentists a quick, practical overview of today’s surgical options, when to consider them, and what new technologies are improving outcomes.
What is Surgical Periodontal Therapy?
Surgical periodontal therapy includes procedures which are done to clean deep infected areas, reshape unhealthy bone, reduce pocket depth, and help the gums reattach to healthier positions. The goals are:
- Stop disease progression
- Reduce bacterial infection
- Improve long-term tooth stability
- Promote regeneration where possible
Types of Surgical Periodontal Therapy
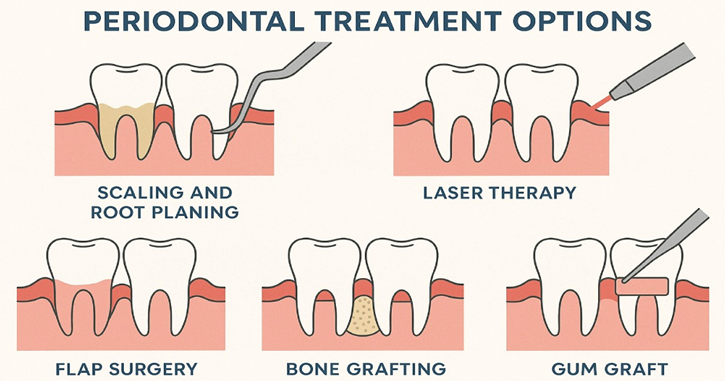
- Flap Surgery: Gums are gently lifted to clean deep deposits and reshape bone where required.
- Osseous Surgery: Removes bone irregularities and creates a healthy bone.
- Gingivectomy: Removes extra or diseased gum tissue, especially in cases of gum overgrowth.
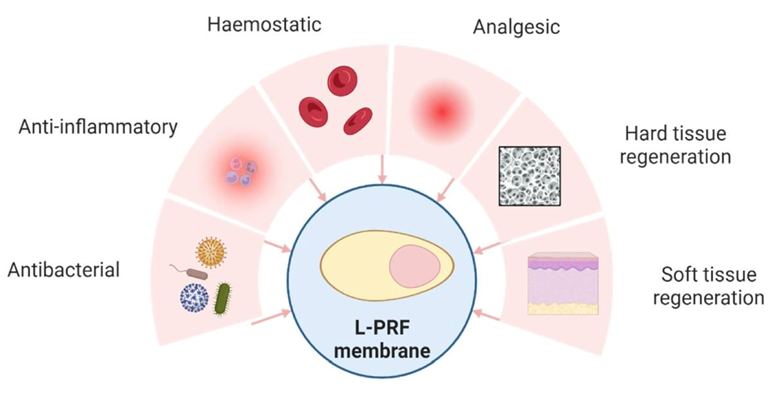
- Regenerative Surgery: Uses bone grafts, collagen membranes, PRF
- Minimally Invasive Microsurgery: Uses microscopes and tiny instruments for faster healing and less discomfort.
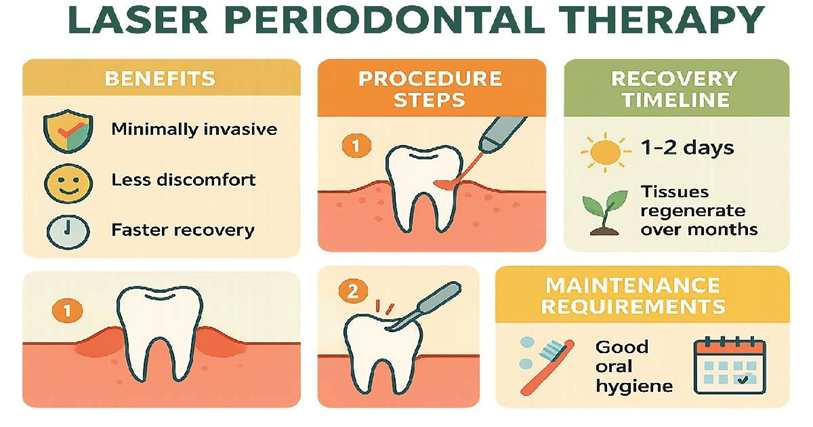
- Laser Periodontal Surgery: Targets diseased tissue with less bleeding and improved results.
- Guided Periodontal Surgery: Involves 3D planning and printed guides for high precision in difficult cases.
Benefits of Surgical Periodontal Therapy
- Lower pocket depths
- Improved periodontal stability
- Reduced inflammation and infection
- Boost in long-term tooth survival
- Better aesthetics, especially in visible areas

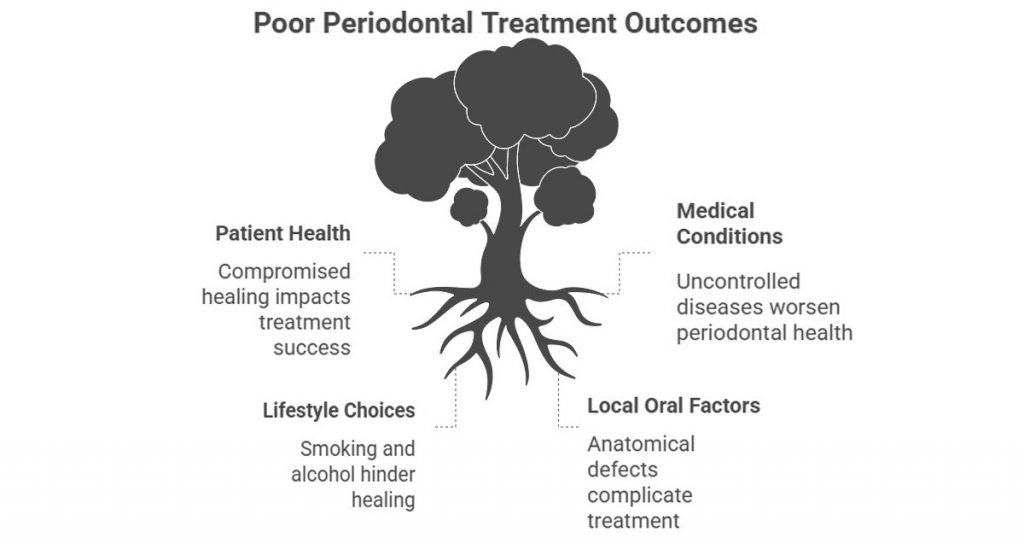
Risk Factors and Case Selection
Selecting the right cases plays an important role in positive outcomes. Here are the important factors:
General Patient Risk Factors
- Older age or compromised healing
- Poor diet, high stress levels, weak immunity
- Bad oral hygiene habits
- Previous history of severe periodontitis
Medical Conditions That Increase Risk
- Uncontrolled diabetes
- Hormonal imbalances
- Obesity
- Medications that cause gum enlargement
- Immune-related disorders
Lifestyle-Related Risks
- Smoking (major negative impact on healing)
- Heavy alcohol use
- Irregular dental check-ups
Local Oral Factors
- Deep anatomical defects
- Furcation involvement
- Overhanging restorations
- Calculus deep under gums
- Occlusal trauma
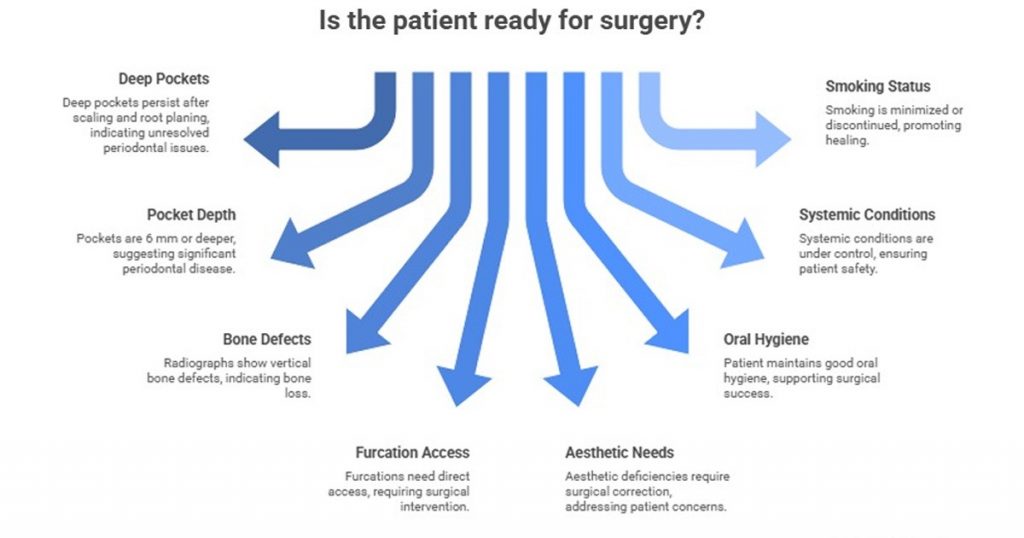
Case Selection Checklist
A patient is generally ready for surgery if:
- Deep pockets persist after scaling and root planing
- Pockets are 6 mm or deeper
- Radiographs show vertical bone defects
- Furcations need direct access
- Aesthetic deficiencies require surgical correction
- Patient maintains good oral hygiene
- Systemic conditions are under control
- Smoking is minimized or discontinued
Patients with hopeless teeth, extreme mobility, or poor compliance may not benefit from surgery and may require extraction instead.
New Advancements in Periodontal Surgery
Modern periodontal therapy has advanced significantly and that includes the following:
Digital & AI-Assisted Diagnosis
- AI tools help detect bone loss earlier
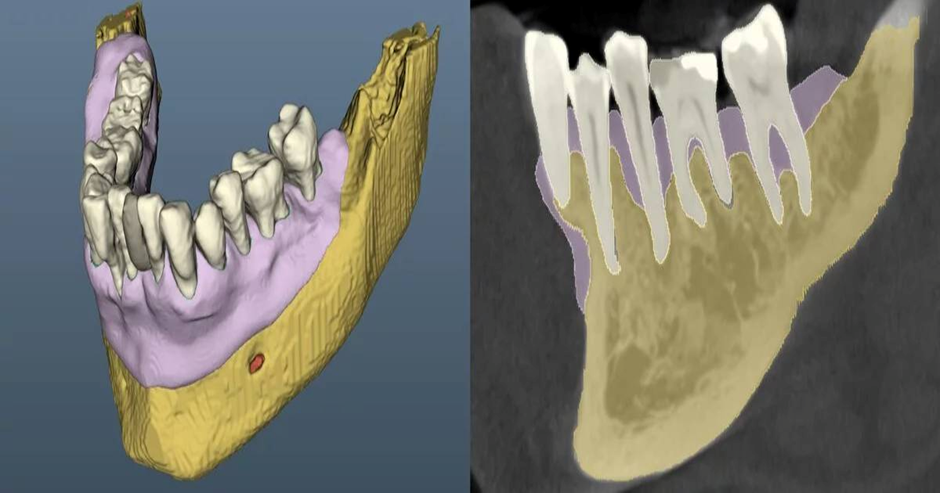
- CBCT imaging offers accurate 3D mapping of periodontal defects
- Digital scans replace traditional impressions

3D-Guided Periodontal Surgery
- Custom surgical guides improve flap design and graft placement
- Higher accuracy reduces chair time and enhances predictability
Biologics and Regenerative Science
- PRF and concentrated growth factors improves healing
- Advanced collagen membranes improve graft stability
- New synthetic grafts offer better integration
Minimally Invasive Techniques
- Microsurgical tools make incisions smaller and more controlled
- Better esthetics and faster recovery for patients
Laser Therapy
- Less bleeding and inflammation
- Selective removal of diseased tissue
- Supportive role in regeneration
Smart Periodontal Tools
- Ultrasonic devices with feedback systems
- Specialized tips for deeper access
- Improved precision with minimal trauma
Together, these advancements have made periodontal surgery more comfortable, more predictable, and more acceptable for patients.
Complications to Expect
Although modern techniques have reduced complication rates, some issues may still arise:
Common Post-Surgical Issues:
- Mild bleeding
- Swelling
- Discomfort or pain
- Temperature sensitivity
- Slight bruising
- Limited mouth opening
- Temporary change in taste
How to Manage Common Complications
- Bleeding: Apply pressure; if prolonged, add a dressing or re-suture.
- Swelling: Use cold packs for 24–48 hours and recommend anti-inflammatory medication.
- Pain: NSAIDs work well; severe pain could indicate infection.
- Sensitivity: Use desensitizing toothpaste or in-office fluoride treatments.
- Delayed Healing: Reinforce plaque control, ensure nutritional support, and check for flap tension.
- Infection: Watch for redness, pus, or fever; treat early with antibiotics and debridement.

Post-Surgical Care Tips for Patients
Give patients simple instructions:
- Use prescribed rinses exactly as instructed
- Keep brushing gentle and do not skip cleaning
- Eat soft foods for a few days
- Avoid smoking during healing
- Take all medications as prescribed
- Attend scheduled follow-up visits

These simple steps make a major difference in healing quality.
Conclusion
Surgical periodontal therapy remains one of the most effective solutions for advanced periodontal disease. With improved digital tools, biologics, lasers, and minimally invasive techniques, dentists can now offer more predictable, comfortable, and long-lasting outcomes. Choosing the right cases, understanding risk factors, and knowing how to manage complications all contribute to successful results. This 2025 update gives you a clear, practical, simplified overview—ready to use in daily practice.
For earlier stages of gum disease, non-surgical periodontal therapy still plays a crucial foundational role before considering surgical intervention.
FAQ’s
Surgery is recommended when deep pockets (usually 6 mm or more), bone defects, or furcation involvement do not respond enough to scaling and root planing.
Yes. Smoking slows healing, reduces blood flow, and lowers the success rate of regeneration. Smokers heal slower and have higher complication risks.
Patients with vertical bone defects, good oral hygiene, controlled systemic health, and non-smokers usually show the best regenerative results.
Most patients resume normal daily activities within 24–48 hours, but strenuous exercise and hard foods should be avoided for a few days.
Maintenance every 3–4 months is ideal to protect the surgical results, control plaque, and monitor healing long-term.



No Comment